Your Heart and Your Sleep
Estimated reading time: 17 minutes
“They died in their sleep…”
It’s World Heart Day (29th Sept). So, in this post, about heart disease and obstructive sleep apnoea, I look at the risk factors and warning signs for both conditions, and review the experts’ latest scientific statements.
To tell you simply, what they advise you to do, so you can live a longer and healthier life.
Is it possible to die from sleep apnoea?
Kind of a yes. Indirectly…
While according to the World Health Organisation, Heart disease (cardiovascular disease CVD) is the single biggest killer worldwide our ageing and overweight population, predispose us to obstructive sleep apnoea.
So it is significant when the American Heart Association release an imaginatively titled Scientific Statement:
“Obstructive Sleep Apnoea and Cardiovascular Disease: A Scientific Statement From the American Heart Association“
On the back of that, some reasonable questions are:
- Who gets Heart disease?
- What is Obstructive Sleep Apnoea (OSA)? And ‘So what?’
- Why is the Scientific Statement a big deal?
To answer these, I’ve split this article into three parts:

Part One
Heart disease: Who gets it?
Cardiovascular Disease – the Killer we know
The World Health Organisation state that ischaemic (reduction in blood flow) heart disease is responsible for 16% of the world’s total deaths.
They provide this happy chart:
While who gets heart disease is not yet clear, there are known risk factors. Minimising these may reduce your chances of developing heart disease.
According to the NHS, the main risk factors for heart disease include:
- High blood pressure (hypertension)
- Smoking
- High cholesterol
- Type II diabetes
- Inactivity
- Obesity
- Family history
- Ethnic background
While some risk factors for heart disease you can do nothing about, others you can control e.g.: quitting smoking and losing excess weight.
Shockingly, 64% of adults in England are either overweight or obese so losing excess weight has to be considered a top tip.
Losing excess weight would appear a really good idea when as a risk factor it is feasible to address, and the improvement in terms of quality of life and reduced likelihood of developing a chronic disease is abundantly clear.
Figure 2 below, illustrates how in the US the situation is dramatically worsening.
Indeed, Centers for Disease Control and Prevention (CDC) data from 2018 shows that a frightening 73% of US adults are either overweight or obese.

High blood pressure (BP) is one of the most important risk factors for cardiovascular disease (CVD). US data from 2018 shows a reversal of a previous downward trend. See figure 3.
Other risk factors for developing heart disease:
Heart disease is more common in men over 50. Dietary choices and excessive alcohol consumption can increase your risk of developing high cholesterol and high blood pressure, and aggravate your weight management efforts.
In the UK, heart disease was the leading cause of death for men (13.1% of all male deaths), while the leading cause of death for women was actually Dementia and Alzheimer disease (16.1% of all female deaths).

Indeed, approximately 10% of the UK population (around 7.6 million people) are living with a heart or circulatory disease:
- 4 million men
- 3.6 million women
While in the US, the leading cause of death is similar to the UK at 13%.
So that’s the grim news about heart disease.
But what is obstructive sleep apnoea and how do these two conditions relate?
Keep reading and I will explain:
Part Two
Obstructive Sleep Apnoea: The (not so) Silent Deadly Accomplice
According to the American Academy of Sleep Medicine, [PDF download]
“sleep is essential to health”
so if you don’t know much about sleep apnoea, it’s time to learn:

What is Obstructive Sleep Apnoea (OSA)?
Obstructive Sleep Apnoea (spelt ‘apnea’ in the US) is a life-threatening disorder that causes you to stop breathing repeatedly – often several hundred times per night – during your sleep.
Sufferers typically snore and are sleepy in the day, as they must wake up to breathe.
Sleep apnoea complications include:
Excessive daytime sleepiness
Aggravated management of high blood pressure and heart problems
Difficulty controlling Type 2 diabetes
May lead to metabolic syndrome
Complicates anaesthesia
Liver problems
Sleep-deprived partners
OSA – So what?
You will note that the second item in the list above is:
- ‘Aggravated management of high blood pressure and heart problems”.
Which simply means:
OSA is making it difficult for your doctor to manage your high blood pressure/heart problem.
Bluntly:
- You will live longer if your OSA is treated with Positive Airway Pressure (PAP) therapy
- Your heart condition is more difficult to manage if you have untreated OSA
In an analysis from the Sleep Heart Health Study, a Positive Airway Pressure (PAP) prescription was associated with 42% lower incidences of dying among patients with severe OSA, but this risk reduction was not seen until 6 to 7 years of follow-up.
Lisan Q, Van Sloten T, Marques Vidal P, Haba Rubio J, Heinzer R, Empana JP. Association of positive airway pressure prescription with mortality in patients with obesity and severe obstructive sleep apnea: the Sleep Heart Health Study. JAMA Otolaryngol Head Neck Surg. 2019;145:509–515. doi: 10.1001/jamaoto.2019.0281
Signs of Obstructive Sleep Apnoea – Self Test
Now do our Online Snoring Test to see if you show signs of Obstructive Sleep Apnoea / apnea.
Your data isn’t stored, shared or in other ways abused!

Who gets OSA and Why?
Risk factors for OSA include:
- Being male
- Obesity
- Alcohol
- Smoking
- Age
Excess weight is the single biggest modifiable confounder. Indeed, the differences in the way men and women deposit fat (before the menopause) go some way to explain why men are more likely to develop OSA.
How many people have OSA?
OSA is more common than you may think.
In fact, prevalence is increasing due to our ageing population and increasing obesity (we've been over that...).
The OSA Partnership Group propose that:
“Obstructive sleep apnoea (OSA) is more common than you might imagine: perhaps as many as one in ten middle-aged men have it.”
They suggest prevalence for vocational drivers:
"... could be 15–20%.”

The OSA Partnership Group make this OSA prevalence estimate for the UK:
"Thus in conclusion the quoted estimates for the prevalence of any level of OSA (mild, moderate or severe) in the UK could be argued to be 25%, but that only about 5% (1.75 million) would be likely to benefit from CPAP treatment. Presumably a larger number might benefit from other less intrusive treatments such as a dental device or weight loss."

OSA symptoms and diagnosis
- Excessive daytime sleepiness
- Irritability
- Difficulty with weight management
- Depression
- Erectile dysfunction
- Snoring
Your GP cannot diagnose obstructive sleep apnoea. If they suspect you have OSA they will refer you to a sleep unit for further investigation. Sleep units are found in large hospitals in the UK (sadly large parts of the UK do not have direct access).
OSA diagnosis requires an overnight sleep study (usually carried out in your own home) and can only come from a sleep physician (typically a respiratory physician).
OSA treatment options
Current NICE Guidelines https://www.nice.org.uk/guidance/NG202 state that first-line therapy for OSA is Positive Airway Pressure (PAP) therapy.
While an arduous and intrusive therapy, PAP is considered effective at overcoming obstructive apnoea events and restoring sleep. Indeed, I have heard patients report feeling:
“10 years younger”.
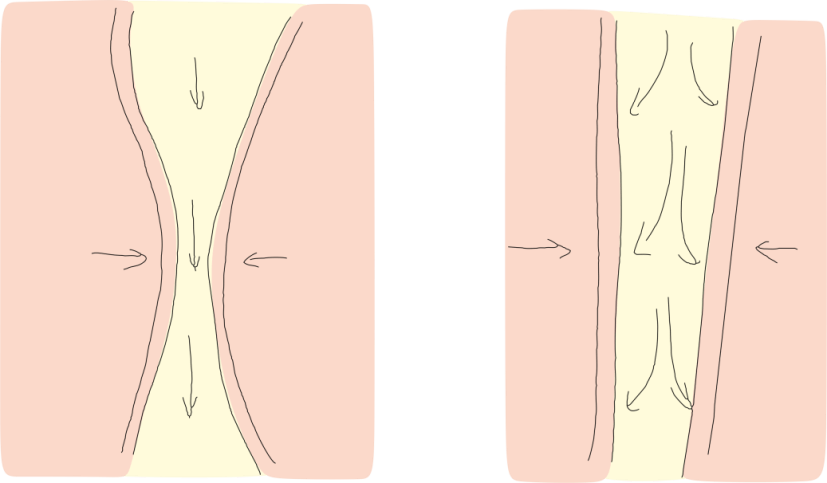
What is PAP and how does it work?
Positive Airway Pressure or PAP therapy is when you wear a mask over your nose (sometimes your mouth and nose) while air (not oxygen) is use to pneumatically splint open your airway. See figure 6.
The OSA Partnership Group propose that less than half the estimated potential patients likely to benefit from PAP (1.75 million) are on treatment.
They continue:
- Presumably a larger number might benefit from other less intrusive treatments such as a dental device or weight loss.
Check out or free information guides for more about the available treatment options for OSA.
Dental devices? Lets take a look at those:

Dental devices: The Second Category of Treatment for OSA:
Custom-made, prescription oral appliances (I am not referring to over-the-counter 'mouthguards') are second line therapy for severe OSA. And they should be brought to your attention when OSA treatment is discussed.
While oral appliance therapy is preferred by patients, difficulty remains evidencing both their effect and patient compliance. As such, when a patient has mild to moderate OSA and comorbidities PAP is considered first-line therapy.
Oral appliance therapy may also be considered for patients with mild to moderate OSA who cannot tolerate continuous positive airway pressure. And some would argue they are first line therapy in this situation.
Check out our Information guides for independent, evidenced-based information about how to choose among these treatment options https://www.snorer.com/information-guides/ and also the role of surgery.

Why get OSA treated?
Apart from living a longer healthier life, you can also look forward to:
- better mood
- less snoring
- less daytime sleepiness
- improved quality of life and work productivity
By now I am sure you appreciate that cardiovascular disease and sleep apnoea are two evils.
But why is the American Heart Associations (AHA) Scientific Statement a big deal?
That's what I look at in Part Three:

Part Three
Why is the AHA Scientific Statement significant?
Impressively, the AHA Statement has been endorsed by no less than 25 medical, scientific, patient, and safety organisations.
They all agree with the medical experts from the American Heart Association (AHA) that:
- Obstructive Sleep Apnoea / apnea (OSA) is an under recognised condition
- Everyone with cardiovascular risk factors or diagnosed heart conditions should be screened for OSA and treated as appropriate
Although this may not sound like it, this Scientific Statement is good news!
Why?

A suspicious relationship...
Th AHA Scientific Statement is good news because, historically, cardiologists viewed the evidence supporting OSA treatment with, let us just say suspicion.
This is where I might upset people…
When I write about heart disease and OSA, and necessarily simplify things, it gets tricky.
Not least because the medical terms and theories are complex (and the research papers, it must be said soporific), but because even the medical experts have divergent views on the relationship between these two chronic diseases.
Coming from an OSA background, I would make these two observations:
- Cardiologists are accustomed to an abundance of exceptionally good clinical proof (their research typically being funded by large pharmaceutical companies, with many patients, and many centres, over many years)
- Data supporting OSA treatment efficacy is typically smaller in scale (some notable exceptions).

Cardiovascular Disease and Obstructive Sleep Apnoea
Contentious or not.
It would seem logical and reasonable to suggest:
If you cannot breathe when you sleep, it is a problem for your circulatory system.
Let me expand on that:
If your heart is struggling because you have heart disease, and you compound this difficulty with sleep apnoea (making your heart work harder to get the remaining oxygen in your bloodstream around your body), while depriving yourself of quality sleep:
It’s a recipe for disaster.
I have a heart condition - could I also have OSA?
If you're reading this and you have heart disease then consult your GP and discuss obstructive sleep apnoea with them.
And if you are in direct communication with your cardiac (heart) department, raise the OSA question directly with them.

What can Health Care Professionals do about OSA?
Get educated: OSA is under recognised
Learn more about Obstructive Sleep Apnoea!
The recent American Academy of Sleep Medicine’s Position Statement went so far as to say :
"….. sleep education should have a prominent place ….. medical school and graduate medical education, and educational programs for other health professionals"
To quote the AHA Scientific Statement:
Despite its high prevalence in patients with heart disease and the vulnerability of cardiac patients to OSA-related stressors and adverse cardiovascular outcomes, OSA is often underrecognized and undertreated ...
They continued:
We recommend screening for OSA in patients with
- resistant/poorly controlled hypertension
- pulmonary hypertension,
- recurrent atrial fibrillation after either cardioversion or ablation.

Calling Community Pharmacists: You're the front line!
Community pharmacists:
Have you considered asking the patient about their sleep?
What about the comorbidities: Has anyone discussed them recently?
We offer pharmacists a completely free online training course about snoring and obstructive sleep apnoea https://snorer.com/pharmacist/
Calling General Dental Practitioners: You can help too
When you take a medical history, why not ask about your patient’s sleep?
"Do you (or your partner) snore?"
It's not just about making 'anti-snoring devices'. We provide independent, online Continuing Professional Development to help you:
- screen and recognise obstructive sleep apnoea
- know how and when to safely provide oral appliance therapy
Dentists: Free Stop Snoring Course

Snorers (and their long-suffering partners)
The first thing to do when snoring is a problem is to consult a sleep-trained pharmacist or your General Medical Practitioner if you cannot find one.
Read (and bookmark) our Definitive How to Stop Snoring Guide and appreciate there are no magic 'snore cures'.
If you've begun the process already, and need to know how to choose among the prescription treatments, then our free information guides will help you in an independent, jargon-free and evidenced based way.
References
[accessed 23rd June 2021]
UK hypertension stats
[accessed 23rd June 2021]
UK stroke stats
Over 113,000 individuals suffer a stroke each year in the UK, and there are around 1 million stroke survivors currently [1,2]. These numbers are increasing due to population ageing and because treatment improvements lead to better survival rates. The number of strokes each year in Europe is projected to increase by 34% between 2015 and 2035 [3].
https://academic.oup.com/ageing/article/49/2/277/5707457
[accessed 23rd June 2021]
UK heart stats
Over 113,000 individuals suffer a stroke each year in the UK, and there are around 1 million stroke survivors currently [1,2]. These numbers are increasing due to population ageing and because treatment improvements lead to better survival rates. The number of strokes each year in Europe is projected to increase by 34% between 2015 and 2035 [3].
https://www.bhf.org.uk/what-we-do/news-from-the-bhf/contact-the-press-office/facts-and-figures
[accessed 23rd June 2021]
UK obesity
28.0%
28% of adults in England are obese and a further 36% are overweight. This briefing provides statistics on the obesity among adults and children in the UK, along with data on bariatric surgery and international comparisons.
https://commonslibrary.parliament.uk/research-briefings/sn03336/ [accessed 23rd June 2021]
https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2019 [accessed 23rd June 2021]
American Heart Association document
Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE, Somers VK; on behalf of the American Heart Association Council on Clinical Cardiology; Council on Peripheral Vascular Disease; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Stroke Council; and Council on Cardiovascular Surgery and Anesthesia. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021;143:e•••–e•••. doi: 10.1161/CIR.0000000000000988
[accessed 22nd June 2021] available here: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000988
Who gets OSA?
Johnson DA, Thomas SJ, Abdalla M, Guo N, Yano Y, Rueschman M, Tanner RM, Mittleman MA, Calhoun DA, Wilson JG, et al. Association between sleep apnea and blood pressure control among Blacks. Circulation. 2019;139:1275–1284. doi: 10.1161/CIRCULATIONAHA.118.036675 https://pubmed.ncbi.nlm.nih.gov/30586763/ [accessed 9th July 2021]
Sleep Foundation: Sleep apnea and Heart disease
https://www.sleepfoundation.org/sleep-apnea/sleep-apnea-linked-heart-disease [accessed 23rd June 2021]
Sleep Heart Health Study
The Sleep Heart Health Study (SHHS) was supported by National Heart, Lung, and Blood Institute cooperative agreements U01HL53916 (University of California, Davis), U01HL53931 (New York University), U01HL53934 (University of Minnesota), U01HL53937 and U01HL64360 (Johns Hopkins University), U01HL53938 (University of Arizona), U01HL53940 (University of Washington), U01HL53941 (Boston University), and U01HL63463 (Case Western Reserve University). The National Sleep Research Resource was supported by the National Heart, Lung, and Blood Institute (R24 HL114473, 75N92019R002).
How does sleep affect your heart?
https://www.bhf.org.uk/what-we-do/news-from-the-bhf/news-archive/2019/november/sleep-and-heart-and-circulatory-diseases [accessed 29th June 2021]
Sleep is essential to health: An American Academy of Sleep Medicine position statement https://aasm.org/advocacy/position-statements/sleep-essential-health-american-academy-sleep-medicine/ full statement: https://jcsm.aasm.org/doi/pdf/10.5664/jcsm.9476 [accessed 29th June 2021]