

How to prescribe oral appliances for snoring (Ultimate Guide 2021)
Estimated reading time: 36 minutes
This Ultimate (and free) Guide for dentists, about oral appliances for snoring, will show you exactly how and when to prescribe them.
Supplemented with multiple real-life examples, downloads, videos, photos of impressions and 13 intra-oral images.
The best part? If you’re a UK dentist, I will show you how to prescribe oral appliances for snorers without a prior medical diagnosis (and stay indemnified).
Sound good? Let’s dive right in…
Peer review and about the Author

Lucy Ash (Director at Somnowell. Ltd) Director
An excellent resource for both, snorers and healthcare professionals.
10/10/2018
Looking into snoring solutions can be an intimidating process, with so many different options and treatments available. The How to prescribe oral appliances for snoring: Ultimate guide provides in-depth, impartial advice, looking at all the options available, so the practitioner can offer the best service. Well done!
Click to jump to each chapter:
Before we begin… is this you?
A patient has asked me about an Anti-Snoring Device…
STOP.
Unless you’re sleep-trained do NOT prescribe an anti-snoring device.
- You’re not insured (both the Dental Defence Union and Dental Protection Ltd. have position statements on this)
- You may delay your patient’s diagnosis by inadvertently disguising their symptoms: snoring may be a symptom of obstructive sleep apnoea (OSA) and the first-line therapy for OSA is not an oral appliance
I’ve received a referral (patient has sleep apnoea): Now what?
STOP.
While you’re medico-legally ‘OK’ to prescribe an anti-snoring device (the patient has a medical diagnosis and has been referred to you for oral appliance therapy) ask yourself:
“Do you feel sufficiently informed to treat?”
Intrigued? Read on…
CHAPTER 1:
Finding suitable patients
Starting right now, I’ll show you how to find enough patients, to make a fulfilling business from helping snorers.
Beginning with networking, referrals and building your credibility, we then navigate how to accelerate the process through screening and recognition (I will also cover diagnosis).

Finding patients
Helping someone stop snoring, I’m sure you’d agree, is a great aim. Happily, the market for oral appliance therapy for snoring (i.e. prescription, custom-made anti-snoring devices) continues to grow.
Indeed, 20% growth in European unit sales (2017) was reported by one of the few listed companies1 that provide such details.
So, its perhaps surprising then, that in my experience, dentists get very excited, train how to prescribe oral appliances for snorers… and then….
Nothing.
Nothing at all.
If you’re reading this, then maybe you have a snorer in mind (you or your other half perhaps?).
Well you’ve found one snorer, so how hard can it be, to find some more?
After all, it seems just about everyone snores…2
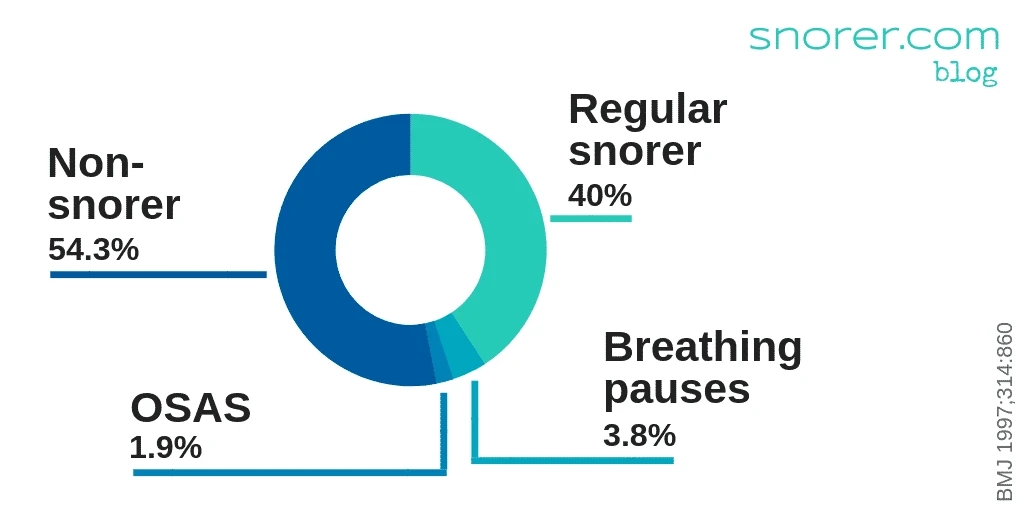
Perhaps a slight exaggeration to say EVERYONE snores, however, in a telephone interview of 4972 people (UK population sample, aged 15 -100 yrs) 40% reported snoring regularly and 3.8% reported breathing pauses during sleep. BMJ, 1997; 314:860 (Ref. 2)
Yet, dentists once sleep-trained either:
- Don’t know how to find these snorers
- Or perhaps it’s just too darn hard (or slow) to make a real go of it
Why is that?
(Don’t worry – I will tell you why – and how to get snorers knocking on your door).
How to receive referrals of snorers?
Dentists around the world are facilitators in sleep medicine. They facilitate provision of a therapy for a sleep and respiratory condition:
- Snoring (and Obstructive Sleep Apnoea / Apnea).
The choice of treatment (in this case a mandibular repositioning appliance or MRA) is not made by them.
Which is not such an alien situation as it may at first appear…
For instance:
You may as part of your oral health assessment (with training) suspect the patient has an oral tumour and proceed to refer them for expert assessment, diagnosis and a treatment plan.
Perhaps you’re involved in the long-term management of the patient?
Treatment for snoring or OSA follows diagnosis, and the diagnosis of obstructive sleep apnoea / apnea (OSA) is the exclusive preserve of the Consultant Respiratory Physician (after amongst other things an overnight sleep study) – but we’ll get to that in a moment.
It might seem obvious but to receive referrals, you need to be known to the referrer!

JARGON ALERT!
Oral Appliance, Device, Mouthpiece, ‘Gumshield’, Splint…
MRA (Mandibular Repositioning Appliance)
MAS (Mandibular Advancement Splint)
MAD (Mandibular Advancement Device)
MRD (Mandibular Repositioning Device)
These are different names (acronyms) for the same thing: an oral appliance which holds the lower jaw forwards to improve breathing while asleep.

JARGON ALERT!
A sleep study is an overnight test that (while the patient sleeps) includes measurements of oxygen saturation, body position and the amount of effort required to breathe.

When can dentists treat snorers?
Snoring may be a symptom of OSA, in which case the sleep-trained dentist is faced with a situation that is more or less delineated by this extract from the American Academy of Sleep Medicine’s Clinical Guideline3 (yes, OK, this is a US Guideline but it’s broadly similar to what’s found in other parts of the world and it makes my point clearly enough):
The presence or absence and severity of OSA must be determined before initiating treatment in order to identify those patients at risk of developing the complications of sleep apnea, guide selection of appropriate treatment, and to provide a baseline to establish the effectiveness of subsequent treatment.
This is an ideal time to define obstructive sleep apnoea:
What is Obstructive Sleep Apnoea?
Obstructive sleep apnoea (OSA) is a condition where breathing repeatedly stops during sleep4, because the upper airway behind the tongue, has narrowed or collapsed. Sufferers commonly snore.
What are the symptoms of Obstructive Sleep Apnea Syndrome?
Obstructive sleep apnoea syndrome (OSAS) gives rise to unexplained daytime sleepiness as the dominant symptom. Sufferers experience major adverse physiological changes, due to the recurrent asphyxia and micro-arousals that fragment their sleep.5
Other symptoms include:
- Reduced vigilance
- Difficulty concentrating
- Poor at work, home and driving6 performance
- Snoring
OSAS fragments someone’s sleep to such an extent that they’re unaccountably drowsy and tired when they should be wide-awake.7
How to differentiate between snoring and OSA?
This is the crux of the issue.
Differentiating between OSA sufferers who snore (who would benefit and most likely comply with a Positive Airway Pressure or PAP device) and ‘simple’ benign snorers, who would be most appropriate for an oral appliance is what sleep units ‘do’.
You need to leave this to the professionals in the sleep unit. (Unless you’re a dentist in the UK – we’ll get to how this works later).

JARGON ALERT!
PAP = Positive Airway Pressure therapy.
This is the best option for severe obstructive sleep apnoea (OSA).
Learn more about PAP therapy with this ‘How to choose: PAP therapy‘ ↗ Guide

How to get referrals from the Sleep Unit, ENT and MaxFac departments?
Active networking is not for everyone.
However, as a sleep-trained dentist wishing to receive referrals, you will need to network with:
- Your local sleep unit
- The ENT department
- The Oro-maxillofacial department

The departments in your local hospital (listed above) need to be aware of your existence and training, for you to receive referrals of patients, in the following circumstances:
- When snoring patients do not merit treatment with PAP therapy or sleep apnoea patients have refused or failed with it
- ENT approaches have not been successful or require concurrent oral appliance therapy
- Oro-maxillofacial surgery is not considered appropriate

It certainly won’t hurt to write to them, yup, good ol’ snail mail.
Also, make sure you attend any continuing education events the units may run, join the available professional societies and go to the national sleep conferences (I can see a joke here – but I’m not going there)
There’s no way around it:
It will take some time and effort.
This rather passive, ‘wait and see’ approach as to when you can prescribe an oral appliance for snoring, is globally applicable – with one unique exception (in the United Kingdom):
Which I hinted at earlier and can now reveal…
How to screen and recognise obstructive sleep apnoea (OSA)
Sleep-trained dentists in the UK, using the British Society of Dental Sleep Medicine (BSDSM) pre-treatment screening protocol8, may screen and recognise obstructive sleep apnoea (OSA) symptoms (and refer for further investigation).

What this means:
You can train to identify snorers who can be treated safely with oral appliances, without a prior medical diagnosis.
Which is a globally unique situation (to the best of my knowledge).
Screening for obstructive sleep apnoea?
Dentists screen for oral conditions every day.
Call it an ‘oral health assessment’ if you like, whether you’re screening for gingivitis, caries or an oral tumour… screening for a condition is simply looking for the warning signs, while it’s in its infancy.
The idea of course, is that a condition in its early stages may be more easily treated or managed.
Can I screen for obstructive sleep apnoea?
Screening for OSA is no different to the screening (sorry oral health assessment) that you do routinely.
The conversation begins by adding the important question:
“Do you snore?”
to your medical history questionnaire. If you ask this question, then I’m sure you will be amazed how many snorers you discover – and how many want to talk to YOU about their condition.
Sleep-trained dentists may recognise (and I use the word ‘recognise’ intentionally) symptoms of obstructive sleep apnoea, including:
- Daytime sleepiness
- Obesity
- A partner witnessing breathing interruptions during sleep
- Awakenings due to gasping or choking fits
- Frequent night awakenings to urinate
- Need to sleep sitting up
- Snoring
It’s important to note that UK sleep-trained dentists are not diagnosing.
They are assessing according to an agreed, published protocol and acting within the bounds of their professional indemnity insurance9, 10 (which is kind of important!).
Unless you’re a sleep-trained dentist in the UK, you need to refer EVERYONE to their GP (primary care physician – PCP) for the doctor to decide who should be referred for a sleep study after which the most appropriate treatment can be discussed. You might well see the patient again for the fitting of an oral appliance.
The Association of Respiratory Technology and Physiology (ARTP) Standards of Care document, cites the British Society of Dental Sleep Medicine’s pre-treatment screening protocol (as published in the BDJ May 2009, by Prof. John Stradling FRCP and Dr Roy Dookun BDS).
These two documents make up the ‘rules of the game’ for UK sleep-trained dentists.
We’ll get into this some more later (Chapter 4 – What training do I need?).
The benefits of dental screening and recognition of sleep apnoea
OK, so you can’t immediately prescribe an oral appliance for snoring.
But the snorer you refer to their GP (or Primary Care Physician if you prefer) effectively becomes your ‘sales person’. The patients you push through the system the right way, then help to reinforce your networking.
The sleep unit medics will think:
“Here is a responsible, informed professional – lets send our patients to them.”
Tick.
Diagnosis of snoring and / or obstructive sleep apnoea (OSA)
As I said in the paragraph ‘Screening and Recognition’ above, the diagnosis of OSA and what is known as ‘simple’, ‘benign’ or ‘anti-social’ snoring is not something a dentist can do.
Here’s the pertinent extract from Dental Protection Ltd’s position statement (a UK-based professional indemnity insurer):
The diagnosis and treatment of OSA, other sleep disturbances or snoring conditions does not fall within the definition of the practise of dentistry and therefore falls outside the scope of assistance normally provided by Dental Protection. However, dentists can have an important role in the screening of patients for signs and symptoms which may predict the presence of OSA.
Consequently, determining that your patient ‘just’ snores and prescribing an oral appliance for snoring, is likely to get you into ‘hot water’.
And it would comprehensively obliterate any credibility you’ve built up, with all your networking and screening efforts.
Sleep-Related Breathing Disorders: The Dentist’s Role
There is an expectation that patients see their GP at a frequency, based upon their age and needs.
For example, a new mother would perhaps see their GP regularly (say once a week – a month), whereas young adults perhaps less so (once every few years – or only as necessary). And so on.
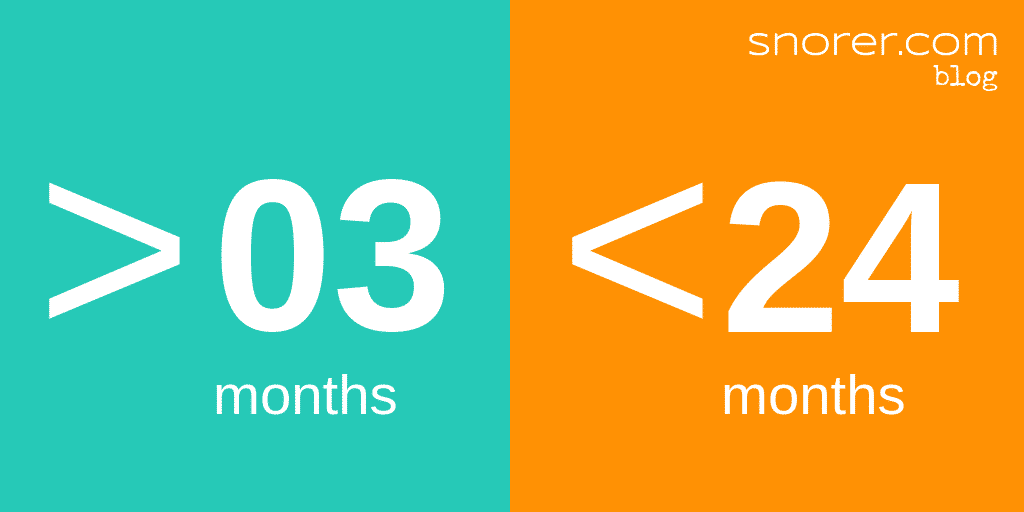
Dentists on the other hand, generally see their patients (and look in their mouths) at defined and comparatively frequent intervals.10 i.e. more than 3 months and no more than 24 months apart.
As such, dentists are ideally placed to play 4 critical roles12:
Treating adults with oral devices for snoring and mild to moderate OSA to slow the progression of the disease
Identifying patients at risk (both children and adults) by looking at their upper airways on a regular basis
Treating children with rapid maxillary expansion and avoiding deleterious orthodontic treatments
Recognising the need for bimaxillary osteotomy among young adults with a need for maxillofacial correction
Top tip: Sleep-related breathing disorders: Dentists are ideally placed to play 4 critical roles.
So, as a UK dentist with dental-sleep medicine training, YOU can become a valued member of the sleep patient care team.
You just need to find patients…
Have signposted snorers making appointments with you.
CHAPTER 2:
What are the dental clinical signs and symptoms of sleep-related breathing disorders?
Picture yourself:
You’re screening performing an oral health assessment and you start to wonder:
“What are the dental signs and symptoms of sleep-related breathing disorders?”
Well, lets have some real-life examples:

What are the dental clinical signs & symptoms of sleep-related breathing disorders (SRBD)?
Let’s have some examples. You may come across these dental clinical signs and symptoms of possible Sleep-Related Breathing Disorders (SRBD).
Including:
Tongue crenulations (scalloped borders) suggesting perhaps both bruxism and that the patient is regularly pushing the tongue forwards against the teeth to open their oral airway.

The development of an anterior or lateral open-bite relationship may result from tongue posturing.
Sleep bruxism may develop or increase (see point 1 above)
Dimpling of the cusps and lingual surfaces of the teeth may be an indicator of related gastroesophageal reflux. Reflux may occur due to ‘pumping’ efforts to breathe bringing up stomach acid.


The development of:
- Orofacial pain
- Temporomandibular joint (TMJ) dysfunction symptoms
- Masticatory muscle fatigue noted on awakening
- Morning headache
These can be related to the positioning of the mandible to open a person’s airway or bruxing after a sleep apnoeaic episode.
During the evaluation of the oropharynx, prominent tonsils, a large uvula, or a narrow or tongue-obstructed airway may be noted.
The patient’s age may also contribute to loss of tone of the pharyngeal muscles.
Evidence of mouth breathing while sleeping may take the form of drying of the surface of the gingiva.
Halitosis
What should I do if I suspect the patient has sleep apnoea?
If your suspicions are aroused, then refer the patient to their GP (in writing) for further investigation. Or if you’re in the UK and you’re a sleep-trained dentist, you should screen for OSA and its comorbidities.
And if you look down a patient’s throat and see this – what does it tell you?
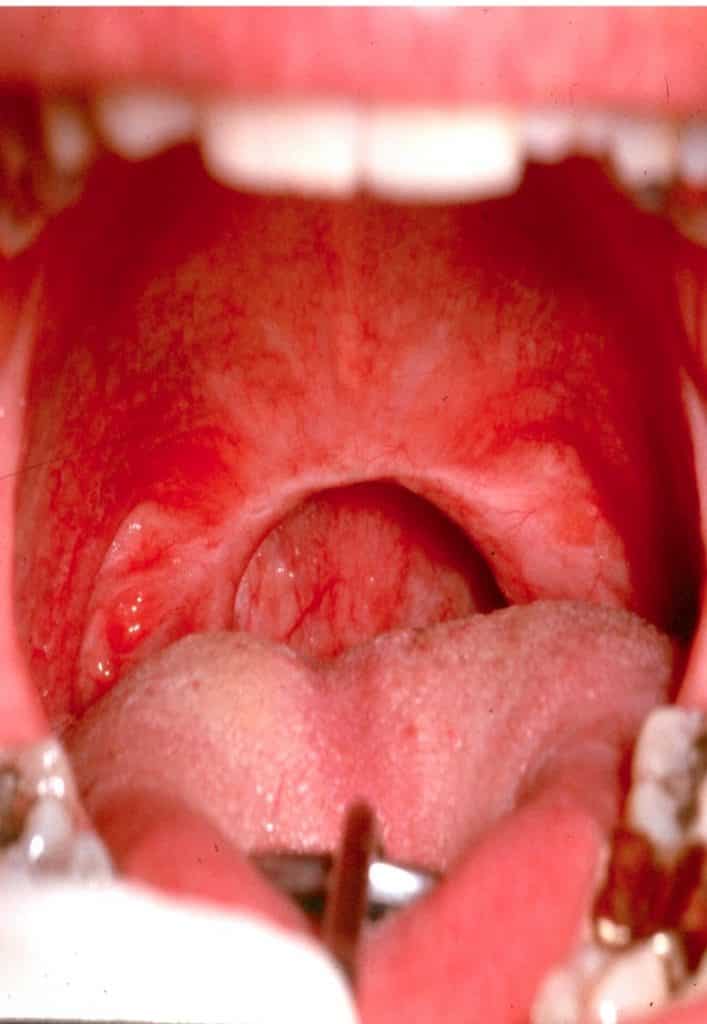
This patient has had a UVPPP (sometimes its written UPPP). This acronym stands for ‘uvulopalatopharynogplasty’ and this is the ENT surgery solution for problem snoring.
Read more about surgery for snoring.
CHAPTER 3:
Can I prescribe an oral appliance for snoring?
Now (at last) we can answer your question:
“Can I prescribe an oral appliance for snoring?”
And this is absolutely about WHEN as a dentist you can prescribe.
Time to put the sickle scaler down.

When to prescribe oral appliances for snoring?
It really is the million-dollar question! So, let’s start positively.
You can prescribe an oral appliance for snoring when:
The patient has been diagnosed by a sleep unit and referred to you for an oral appliance for snoring or obstructive sleep apnoea.
You’re a UK sleep-trained dentist, who has screened for OSA, and is satisfied the snorer is a candidate for oral appliance therapy.
Now back to reality with a bump…
If either of the above 2 conditions are not satisfied, then you cannot prescribe an oral appliance for snoring.
Sorry, I don’t make the rules. (Err… Except I did have a hand in making the rules in the UK… but that’s another story).
Onwards…
In the situation above, the patient has been deemed suitable (from a medical perspective) for an oral appliance for snoring / obstructive sleep apnoea (OSA) and referred to you.
This is now a double prescription situation.
Allow me to explain:
The Consultant Physician has prescribed oral appliance therapy, and YOU as the dentist prescribe which mandibular repositioning appliance (if you consider it dentally appropriate) the patient gets to take home.

JARGON ALERT!
Oral Appliance Therapy is the term for prescription, custom-made medical devices that reposition the mandible to aid breathing while the user is asleep.

JARGON ALERT!
Mandibular Repositioning Appliance, Mouthguard, Device, Mouthpiece, ‘Gumshield’…
MRA (Mandibular Repositioning Appliance)
MAS (Mandibular Advancement Splint)
MAD (Mandibular Advancement Device)
These are different names (acronyms) for the same thing: an oral appliance that repositions the lower jaw to improve breathing while asleep.
Bottom line:
It is down to you as a dentist, to determine if the patient is suitable from your dental, clinical perspective – and then to select the most appropriate oral appliance.
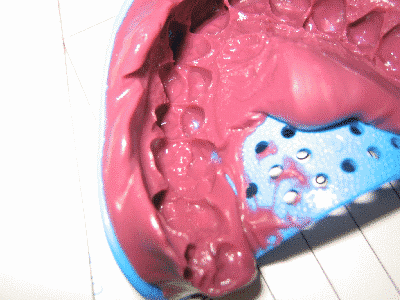
But not like the example shown below:

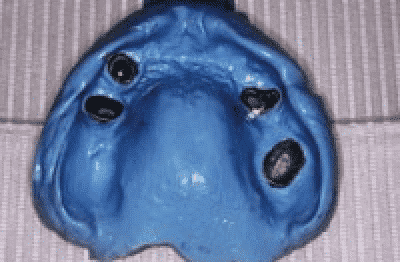
[and yes both impressions are from the SAME patient]
What’s wrong with the above case?
- Insufficient teeth per arch
- Of the remaining standing teeth, they are unevenly distributed around the arch
- Only incisors remaining on the mandible – retaining the MRA and therefore the jaw will be difficult (is this time to consider implants?)
If an oral appliance for snoring were to be prescribed – it would likely prejudice the remaining teeth.
CHAPTER 4:
What training do I need to prescribe an oral appliance for snoring?
The Financial Conduct Authority defines independence for financial advisers, and uses wonderful terms like:
“non-independent advice”
My point is, that any rational person seeks a whole-of-market view, and treats ‘one brand sales spiel’ with a degree of caution.
Selecting dental sleep medicine training, is exactly the same.

Training to prescribe oral appliances for snoring: What’s required?
Staying with my financial adviser analogy a moment longer, the ‘tied’ financial adviser is, in dental sleep medicine terms:
The ‘one oral appliance for snoring dental lab‘ provided course.
Such a course provides you with:
Insufficient knowledge of a broad range of oral appliances for snoring. Just like any other medical device, mandibular repositioning appliances have indications and contra-indications. There is no ideal or ‘best’ device. It all depends upon the patient.
Professional indemnity insurance risk. Why would you use anything other than an insurer approved way to screen and recognise snorers that are safe to treat with oral appliances (without a prior medical diagnosis)? When selecting education, look out for the British Society of Dental Sleep Medicine’s pre-treatment screening protocol.
What constitutes appropriate dental sleep medicine training?
Happily, in the UK we don’t have to guess what constitutes appropriate dental sleep medicine training. We simply refer to the Association for Respiratory Technology and Physiology’s (ARTP) defined training course content:
Cut to the chase: training to do what again?
Training that means you are confident with the below list:
- You must be sufficiently informed about a range of oral appliances for snoring: their indications and contra-indications
- You’re into lifestyle advice, i.e. stop smoking, quit alcohol, lose weight etc.
- You (or a dental nurse perhaps?) need to record (and monitor for changes) the patient’s:
- Blood pressure
- Height
- Weight
- Neck circumference
- You will ideally have examples of different MRA to demonstrate to the patient
- You must explain the risks and benefits: and it’s a good idea to provide this advice in writing
- You must ensure you have valid informed consent (grab an example PDF in Downloads)
- You need to explain the possible side-effects and keep master casts to identify tooth movement – and communicate signs of this immediately to the patient
- You have a duty of care to follow-up snorers and sleep apnoeaics alike (as their condition may change over time)
Here are the pertinent lines re: different designs of oral appliance from the same document (they use the acronym MRD – mandibular repositioning device):
1.5 Equipment
There are a variety of custom manufactured MRD designs available. Some designs may be deemed more appropriate for the individual patient after assessment.
1.7.1 ……………. The identification of snoring/OSA predisposing factors needs to be discussed with the patient and along with appliance assessment factors which must also be taken into consideration as these may influence the design of device to be prescribed or even the decision to provide a mandibular repositioning device at all.
Which means (if you undertake independent training and use the BSDSM protocol) you’ll stay on the right side of the professional indemnity insurers’ position statements.
How the professional indemnity insurers position statements help you
Fortunately, the Dental Defence Union8 and Dental Protection Ltd.9 have issued position statements (and of course other insurers will refer to these as the industries benchmarks).
I say ‘fortunately’ because we’re not guessing.
The position statements and ARTP Standards of Care make it crystal clear WHAT constitutes appropriate dental sleep medicine training and what does not.
Here’s the deal:
- Seek comprehensive courses, independent of manufacturer bias – that make you aware of the wide array of oral appliances (and their indications and contra-indications)
- Screen using the British Society of Dental Sleep Medicine’s protocol or frankly you’re asking for trouble.
Of course, it would be rude at this point not to highlight our www.snorer.training on-demand video courses (naturally do all of the above).
CHAPTER 5:
What does the lab need to make an oral appliance for snoring?
You might be wondering:
- “What impressions does the lab need?”
- “What bite registration is required?
- “Errr… How do I record a protrusive bite?”
- “How many teeth are required?”
Fear not.

Lab requirements
Or to put it another way:
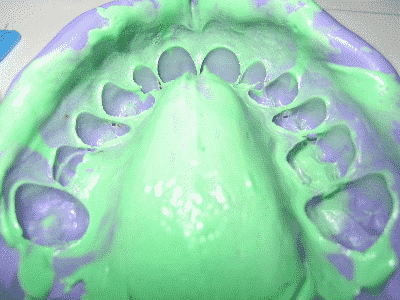
What do good, bad (and plain ugly) impressions look like?
The examples below, illustrate what impressions and the typical protrusive bite registration, should look like. Consult the dental lab (of course) for specifics for each mandibular repositioning appliance you consider.
The impressions shown below are not fictitious.
‘Good’ dental impression for an oral appliance for snoring
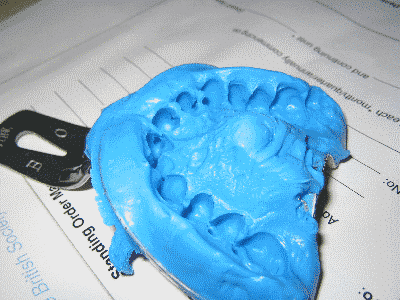
‘Bad’ dental impression for an oral appliance for snoring. (If you look closely you will see a BSDSM standing order mandate!)
‘Ugly’ dental impression for an oral appliance for snoring
What impression material should I use for a mandibular repositioning appliance (MRA)?
Unless your alginate impressions are cast up within the hour, my advice is to use upper and lower fine detail silicone or polyvinysiloxane impressions of all the patient’s teeth. Use a special tray if required.
> Why include ALL teeth in the dental impression for an MRA?
It’s advisable to include the 8s if present, as regardless of whether they are included in the final device, including them aids the lab avoid interference on protrusion and lateral excursions.
> What about sulcal extension?
Pay close attention to the sulcal extension where the device mechanism is to be situated.
What bite registration is needed for a mandibular repositioning appliance?
A protrusive bite registration.
Typically between 50% and 80% of the patient’s maximum protrusion (it may be useful to work back from 100%).
Your protrusive bite registration dictates your choice of oral appliance: Don’t have an oral appliance in mind.
How to record the protrusive bite?
The George Gauge video below (click on it bottom right to go full screen) shows you more about how to take a protrusive bite registration with a product called a George Gauge (you can get these from MRA labs).
[YouTube video used with permission from Great Lakes Orthodontics – who I have no commercial connection with.]

Here’s my non-clinical technical ‘primer’:

How many teeth are required for a mandibular repositioning appliance?
8 teeth per arch (minimum) is a good starting point. However, just as important (if not more so) as the number of teeth, is the arrangement of the remaining teeth:
- You need teeth where you intend to have the titration mechanism
- If there are few molars – incisor sensitivity and ultimately proclined / retroclined incisors will result
So that wraps up general lab requirements. Talk to your lab – they may have their preferences and these may vary for a particular device.
Which brings me neatly to how you choose the ‘best’ oral appliance for your patient:
CHAPTER 6:
How to choose the ‘best’ oral appliance for snoring?
We’ve covered How?, When? and What? now we’ll look at Which?
Which oral appliance for snoring is ‘best’?
When the patient is:
Class II?, Class III? A heavy bruxist? Has edge-to-edge incisors? Has a heavily restored dentition?
Do you mean to say the ‘best’ oral appliance can’t cope?

Which oral appliance for snoring do I prescribe?
There’s a lot of marketing guff about this or that oral appliance for snoring being the ‘best’ one.
The ‘best’ oral appliance for your patient is of course, the one indicated and not contra-indicated.
I’ve written it before and I will write it again:
“There is no ideal (read ‘best‘) oral appliance”
Here are some examples of what I mean:
Situation
Mr X snores. He does not have OSA (referred to you by the local sleep unit), his BMI is 30 but he is otherwise healthy. He is late 30’s, fully dentate, with reasonable oral hygiene and no perio. No evidence of TMD. He is Class II skeletal (mandibular retrognathia) with an acute condylar angle and a ‘step’ between lower 3 and 4. As he protrudes his OVD markedly increases.
Observations
- An oral appliance that crowds his already cramped tongue is contra-indicated.
- As the patient protrudes, an adjustment mechanism between the incisors, may no longer connect
- Gross (and intolerable) vertical opening may develop due to the high condylar angle
- The posterior parts of the oral appliance may impact upon one another
Situation
Mr S snores. He has moderate OSA and is PAP non-compliant (referred to you by the local sleep unit). He sleeps supine (on his back). He is mid 40’s, was a rugby player in his youth and now his BMI is 35 despite exercise. You suspect it relates more to muscle bulk and not so much fat. Neck circumference is 20 inches.
He bruxes and exerts terrific forces on his MRA (which he swears by). He has however found the metal components BREAK. And he has on occasion woken up with the broken part in his mouth.
What do you do?
Observations
Metal components will be work-hardened by his bruxing.
Perhaps consider an MRA where metal components are not subjected to his bruxing forces. Ensure it permits limited lateral movement or be prepared to swap out the metal components at frequent intervals.
Consider offering advice re positional therapy.
Situation
Miss G snores. She does not have OSA (referred to you by the local sleep unit), and she is otherwise healthy. She is mid 30’s, fully dentate, with reasonable oral hygiene and no perio condition. BMI 35. No evidence of TMD. She is Class I skeletal. She has a ‘firm’ incisor relationship (edge-to-edge) i.e. nil overjet / overbite.
Which MRA do you consider is indicated?
Observations
Consider an MRA that neither contacts the labial aspect of the maxillary incisors or lingual aspect of the mandibular incisors to limit and ideally prevent incisor tilting.
Situation
Mrs B snores. She is a new patient. She does not have OSA (referred to you by the local sleep unit), and she is otherwise healthy. She is mid 50’s, fully dentate, with reasonable oral hygiene and no perio condition. BMI 35. No evidence of TMD. She is Class I skeletal. Her incisors have veneers and her molars have bridgework that do not raise immediate concerns.
Which MRA do you consider is indicated?
Observation
Consider perhaps an MRA that is less dependent upon dental retention for its effect.
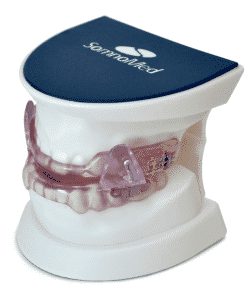
Here are two examples (and there are many more) of oral appliances for snoring with entirely different protrusive mechanisms.
While they both protrude the lower jaw, they have different indications and contra-indications, range of movement, side-effects and frankly costs!
Which one is ‘best!’ Hah!

Why does this matter?
Knowledge of a range of MRAs is vital for you to prescribe the most appropriate for your patient. It gives them the best chance of it working and should minimise side-effects.
Finally, I refer you to the ‘ARTP Standards of Care for MRDs’ document we discussed earlier:
The particular part about:
“…possessing knowledge of a range of oral appliances”.
Sadly, time and again, I’ve witnessed dentists and patients struggling with patently the wrong type of MRA.
- The well-intentioned but misinformed dentist is at a loss. They have nothing else to offer the patient because the ‘one trick pony’ lab they usually rely on, only sells the ‘best’ oral appliance.
- The lab does not have the indicated oral appliance in their portfolio – i.e. they believe their own hype – and are contractually bound NOT to carry competing (shouldn’t that be complementary?) appliances.
How to select the ‘best’ oral appliance for your snoring patient
Earlier I wrote:
“Your protrusive bite registration dictates your choice of oral appliance: Don’t have an oral appliance in mind.”
To elaborate:
The ‘protrusive bite’ informs your decision-making process, when it comes to selecting the indicated oral appliance for your snoring patient.
Buckle up, this gets a little complicated
The objective at this point, is to stay within the adjustment ‘window’ of the mandibular repositioning appliance:
Which is not as simple as it may at first appear…
Let me give you an example:
Assume the (new to MRA) patient’s range of protrusive movement is ~15mm, then consider these points:
- Typical MRA protrusive range is 8-10mm (if more is required then you’re into a remake)
- You might think therefore that an initial protrusive bite that is 5-8mm ahead of centric has you covered
- You know that patient acceptance, during the critical first two weeks of use, may be impaired by an excessive initial protrusion
Now factor in these points:
- With MRA use, the total protrusive range of motion may well increase: Patients don’t normally go around protruding their mandible – their perception of 100% protrusion may well be inaccurate.
- Posterior interference on protrusion: If your initial protrusive bite and final effective (titrated) bite positions are widely divergent, the occlusal surfaces of the upper and lower appliances will require adjustment, typically over the most posterior molars (also bear in mind that gross vertical opening is associated with lower acceptance rates)
- The MRA mechanism does not connect any more: At the limit of MRA protrusion, upper and lower appliances of the ‘hook and screw mechanism between the incisors’ type MRA, may no longer connect.
I did say it was a little complicated.
Moving past the bite registration, what factors influence oral appliance selection?
What to consider when selecting the ‘best’ oral appliance for snoring?
Below is a non-exhaustive list. We’ve discussed the first two points, above:
- Range of oral appliance motion (starting from nil protrusion to enhance acceptance rates)
- Protrusion necessary (how much the patient can protrude – the maximum tolerable)
- Lateral movement (necessity for it?)
- Bruxism (damage to the MRA verging on destruction in a week or less. Or if they brux and the MRA does not permit lateral movement, the MRA may cause an arousal or the patient may simply not wear it).
- Bulk – less is more
- Lip seal – aesthetic considerations and to promote nasal breathing (less vertical opening is associated with higher acceptance and compliance)
- Tongue space invasion – acceptance and frankly effect!
- Incisor contact = incisor sensitivity and proclined / retroclined incisors over time
- Placement of the adjustment mechanism – you need there to be teeth where you want to put the mechanism.
- Material choice (galvanic reaction, different expansion rates of the materials its made from = cracks and remakes, absorption of saliva and cleaning fluids)
- Dexterity of the patient (can they actually adjust it themselves?)
- Control – do you want the patient to be able to adjust it themselves?! Note: an aggressive (read desperate) rate of adjustment of protrusion, WILL aggravate the patient’s TMJs and extend the time it takes to stop snoring
Phew!
Anything else I should look out for?
Yes.
Here are the contra-indications:
What are the contra-indications for an oral appliance for snoring?
Here’s another long list to consider. Does the patient have any of these ‘red flags’?:
- Inadequate oral hygiene
- Poor periodontal condition
- Insufficient teeth per jaw
- Edentulous mandible (some – but not many – MRA designs can be made for edentulous maxillas)
- TMJ locking or other apparent dysfunction
- Inability to protrude more than 5mm from resting jaw position
- Mandibular ‘free end saddles’
- Missing teeth where you would place the titration mechanism
- Short crown height, or ‘pyramid’ shape / under erupted teeth
- Extensive bridgework
- Incompetent or restricted nasal airway
- Severe ‘gag’ reaction
- Unmotivated patient
- Partner motivation for simple snoring (as in they’re not really bothered about the noise themselves)
The presence of these ‘red flags’ does not mean an MRA is out the window. It does mean you need to select the most appropriate oral appliance to prescribe.
Which brings me full circle to:
There is no ‘best’ oral appliance.
The oral appliance has arrived from the lab: Now what?
Once the patient is comfortably inserting (and removing) the MRA themselves, its time to revisit your discussion about seeing them again.
Its important to point out, that for an oral appliance to stop someone snoring, they’re going to need support and encouragement. The first 2 weeks set the pattern for the future.
When do you plan to see them again?
Or perhaps, when should you see them again?
And what’s this about your ‘Duty of Care’?
Top tip: ‘Play’ around with a new oral appliance for snoring BEFORE you see the patient. To work out the adjustments (and know which way up it should be!)
CHAPTER 7:
Titration protocols, follow-up, duty of care
Snorers may need motivating to wear their oral appliance (because it won’t work immediately) and most patients find that it takes time to become accustomed to its presence.
While those with OSA must be followed up rigorously.
What does this actually look like?

What does Subjective and Objective titration mean?
Adjusting the oral appliance’s protrusive position to stop snoring and overcome sleep apnoea, is known as ‘titration’.
Titration comes in two forms:
Subjective
Objective
Subjective titration
Subjective titration means adjustment ceases when the wearer decides (perhaps with the kind assistance of their partner). No further protrusion is required.
Here’s a suggested schedule of follow-up appointments for the benign snorer:
- 3 days from fit a phone call “How has it been…?“
- 7 days from fit an ease, adjust 2mm forwards maximum, reassure
- 3 days later another call “Any improvement?“
- 14 days from fit: adjust 2mm forwards maximum (look for posterior interference)
- Repeat until either snoring ceases or no further protrusion can be tolerated.
Should the patient experience TMJ issues the patient should be instructed to immediately cease wearing the device. Refer them to a TMD expert. An aggressive (impatient) rate of titration WILL bring on TMJ issues in just about anyone.
But what if they’re sleep apnoeaic?
That’s when things get a little more scientific:
Objective titration
Objective titration is when evidence of effect is used, to inform adjustment of protrusion. The patient begins by becoming accustomed to wearing the oral appliance. They then titrate subjectively (see above) and at this point they have a sleep study to see if the MRA is providing effective therapy for their sleep apnoea.
Then a cycle of increased protrusion and repeat sleep studies occurs. Protrusion would cease when one (or more) of these things happen:
- The MRA is deemed objectively effective (great!)
- The physiological limit is reached (not so great)
- Or patient tolerance to the position dictates (tilt!)
Communicate with the patient’s GP and the sleep unit
Write and say thanks for the referral. Advise of your intended treatment plan, your review schedule and ask about repeat sleep studies. Ask about supine sleep position (observed by sleep study) as positional therapy combined with an MRA, can be an effective way to control OSA.
Follow-up and your Duty of Care
As a trained member of the sleep-patient care team, you have a duty of care for both the snorer and the sleep apnoeic patient.
This means you need to monitor the patient for a change in their condition – and not just in their mouth. You need to get the patient reassessed with a view to an alternative or adjunctive therapy. The examples below explain further:
The snorer may:
- Start snoring again – and no further protrusion is tolerable
- Become hypersomnolent (by your assessment informed by the Epworth Sleepiness Scale [see Key sleep terms])
- Experience other OSA symptoms
- Be diagnosed with a comorbidity
- Not improve with increased protrusion
For the diagnosed OSA patient referred to you for prescription of an oral appliance:
Before commencing use they:
- May not be dentally suitable for prescription of an oral appliance
- May consider the risk / benefit analysis (of oral appliance therapy) unacceptable
- They may also find the cost of treatment unacceptable
After commencing use:
- May inadequately respond to protrusion when measured objectively or subjectively
- They may discontinue use and / or fail to attend
The diagnosed OSA patient in the situations above needs to revisit the sleep unit. You need to write to the GP and communicate what has (or hasn’t) happened.
Longer-term follow-up
Longer-term, tooth movement WILL occur. There is no point in dressing this up.
How important is that tooth movement?
Well that’s another thing:
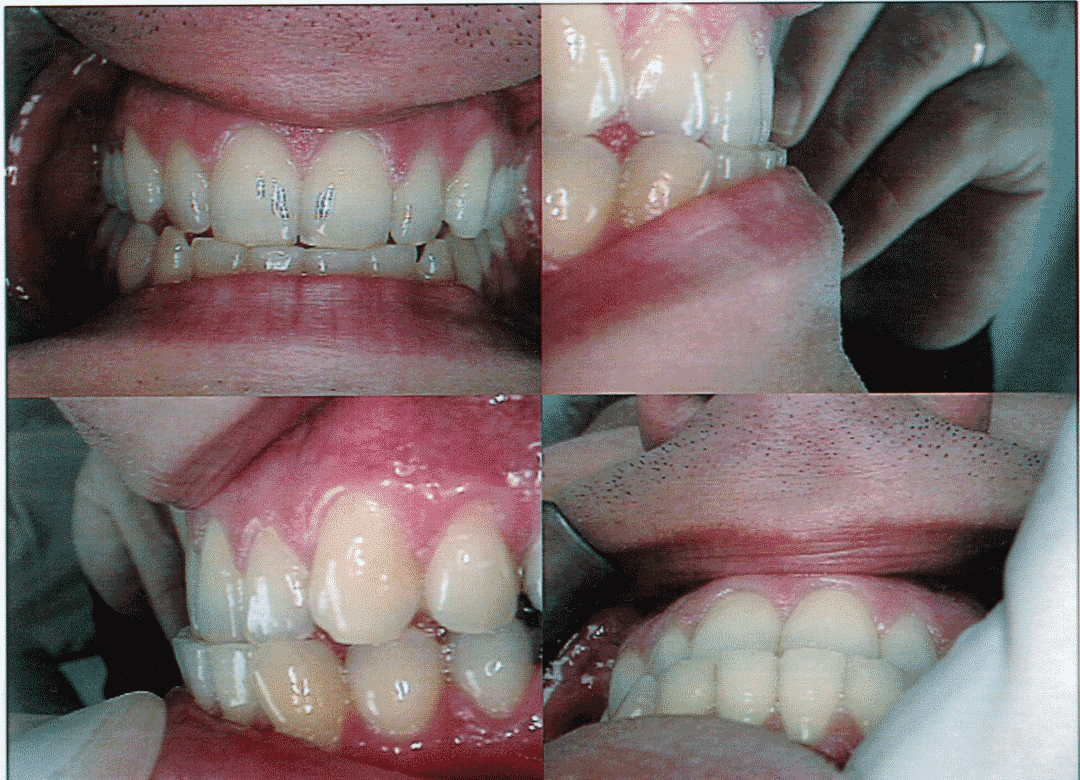
The pictures above are after 21 months of nightly use of an oral appliance for snoring, the patient’s occlusion now appears as an anterior crossbite with an anterior displacement of approximately 2.5mm. These post-treatment photos were taken after three weeks of non-use.
Keeping tooth movement in perspective
It is vital to keep tooth movement, as a result of mandibular repositioning appliance wear, in perspective.
As dental professionals we may be shocked at undesired orthodontic tooth movement. But you may be hard-pressed to extract the effective oral appliance from the patient on the grounds of a tilted incisor!
Points to note here:
- Post-wear exercises e.g. chewing gum in the shower can help the mandible to return to its ‘normal’ position.
- The patient had minimal (if any) overbite before MRA use: an overbite is considered ‘protective’.
Your Duty of Care to both snorers and sleep apnoeaic patients
As a trained member of the sleep patient care team you have a duty of care. Not just to recognise when to treat or refer new patients.
Certainly, you understand the necessity for follow-up of OSA patients, but its important to identify when an MRA is:
- No longer effectively treating the (apparently benign) snorer
- The patient has reached their physiological or maximum tolerable protrusion. Their condition as changed: for example with age, weight gain and lifestyle changes etc.
These patients need your help.
They need you to recognise the change in them (that they may not see themselves) and refer them for further investigation at a sleep unit.
CHAPTER 8:
FAQs and resources
This Guide wraps up with an FAQs and resources section.
Have a question that isn’t answered in our FAQ? Then let us know! contact@snorer.com
If we don’t know the answer – we’ll find out if at all possible! – And also add it to the list:

MRAs aid breathing while the patient sleeps, through anterior repositioning of the lower jaw. There is also an optimum vertical opening.
Is it really: Airway versus Occlusion?
Yes and No.
Yes, long-term use of MRAs will result in occlusal change.
Tooth movement is more likely when:
- MRAs do not fully utilise the canines and molars (these may be more resistant to movement induced by lateral load)
- The number and distribution of teeth is less than ideal
- The MRA design loads the incisors (this will result in retroclined maxillary incisors and proclined mandibular incisors)
Factors that protect against and may limit tooth movement include:
- Post-wear exercises
- An overbite (edge-to-edge incisors are prone to incisor tilting)
- MRA designs that limit the load applied to the incisors
My patient has sleep apnoea and is struggling with PAP – when can I make an oral appliance for them?
When the referring Physician decides. In this circumstance, communicate with the GP and the sleep unit. Explain what is happening, your concerns (i.e. they may use an OTC product) and offer your assistance.
Compared to what? Generally speaking, patients that use prescription custom, adjustable MRAs, use them every night, insert them as they go to sleep and wear them until they wake up.
However, for the sleep apnoeaic patient, the MRA may be less effective (measured using overnight SpO2 saturation) yet used more frequently than PAP therapy (both more hours and more nights a week).
Which therapy is better?
Yes. While MRA designs vary, patients will find a way.
Further, you may wish to retain control of adjustment (see titration).
Patients may adjust the position in error (typically rapidly increase protrusion) and create TMJ issues that prevent use until the joint has recovered. Ultimately delaying effective therapy.
By now you see there is a role (and therapy) ideally suited to the General Dental Practitioner.
It is your choice: do you want to help your patients in this way?
HMRC (the UK’s tax man) considers products for snoring, luxury items and demands 20% VAT.
For patients with diagnosed OSA an MRA is zero rated. You may reclaim ‘input VAT’.
OTC oral appliances will damage the patient.
Problems include:
- Delayed diagnosis and effective therapy
- Pain
- Tooth movement or loss due to excessive and uncontrolled lateral loads
- Posterior open bite
- Development of a reverse incisor relationship
- Development of a protruded mandibular posture
If only life was that simple!
The “Law of Diminishing Returns” applies to MRA titration: initially lateral loads are perhaps low (with minimal side-effects) and the effect increases linearly.
However, beyond a patient-defined protrusion, lateral loads significantly increase for non-linear gains in efficacy.
Still further protrusion may cause pain, significant dental side-effects and less effect.
Key sleep terms
- OSA – Obstructive Sleep Apnoea
- OSAS – Obstructive Sleep Apnoea Syndrome
- ESS – Epworth Sleepiness Scale. Patient completed subjective assessment of sleepiness in specified circumstances
- AHI – Apnoea Hypopnea Index. Index of sleep apnoea severity combining apnoeas and hypopneas:
- 5–15/hr = mild;
- 15–30/hr = moderate;
- and > 30/h = severe
- MRA – Mandibular Repositioning Appliance
- PAP – Positive Airway Pressure
- UPPP/LAUP – UvuloPalatoPharyngoPlasty – Laser Assisted UvuloPlasty
Downloads

- Download: Example of an Informed Consent document as a PDF
- Download: Management of sleep apnoea and snoring, suggested guidelines for General Practitioners and other interested medical professionals. As a PDF.
Related posts from our blog
Patient Information Guides
Now, it’s your turn:
Did this Ultimate Guide help?
- Are you inspired?
- Concerned?
- Awake?!
Let me know by leaving a quick comment below right now (scroll down).

References
Snorer.me Signposting™ is a CE marked, Clinical Decision Support System, Software as a Medical Device. The Manufacturer is Snorer.com Ltd.
Created by Adrian Zacher and Emma Easton. All rights reserved.
This page is intended for Healthcare Professionals
This site is intended to provide balanced, scientific, and evidence-based information that is not intended as medical advice. Responsibility for patient care resides with the healthcare professional on the basis of his or her professional license, experience, and knowledge of the individual patient. This resource may include information that has not been approved by the US Food and Drug Administration. For full prescribing information, including indications, contraindications, warnings, precautions, and adverse events, please refer to the approved product labelling.








Hi there,
Truly great article, I must say and the detail you go through in a clearly understandable and user friendly style is something you don’t find too often!
I just had a semi-related question on patients suffering from TMJ/Bruxism and are looking for more affordable alternatives than a guard or splint provided by a dentist – often questions arise about getting a hold of something via a ‘do it yourself’ method with a home impression kit for a custom fitted guard or boiling what is very near to a sports mouthguard. I’ve attached a couple of examples here:
[links to well-known online shopping sites removed]
I just wondered if you could shed some light on whether either of these could be valid recommendations due to the price point for those not willing to spend the cost of a dentist-made guard or splint.
It would be brilliant to hear from you soon and thank you again for the work you continue to put out.
Best wishes,
Roger
Hi Roger, thanks for high praise – its much appreciated. Apologies for the delay replying (CV19 is my excuse!).
So for the record, I must state that I am NEITHER a Doctor nor a Dentist. I can only point to the evidence – which clearly demonstrates that self-diagnosis and self-treatment of any condition is dangerous and if you are experiencing symptoms of bruxism such as jaw joint pain/tenderness, ear ‘stuffiness’, clicking or locking then please consult an expert TMJ dentist.
You ask about the merits or otherwise (citing cost as the main determinant) of OTC ‘bruxism’ devices.
Again I point to the evidence. I would suggest you review this post: https://snorer.com/otc-dental-devices-for-snoring/
Let me know if you have questions and I can probably direct you to someone who can help you.
Cheers
Adrian