Snoring & Obstructive Sleep Apnoea Overview Guide
Author: Adrian Zacher MBA.
Peer reviewed by: Professor Adrian Williams MD FRCP.
Last review: 10 Dec 2021 Next review: December 2023
Download this Overview Guide as a PDF
Written by Adrian Zacher MBA
Peer reviewed by Professor Adrian Williams MD FRCP
In this NHS England’s Information Standard accredited Guide, you’ll learn in jargon-decoded language:
- Why to take ‘snoring’ seriously
- The benefits of treatment
- When a sleeping problem becomes more serious
- What happens when you sleep
- The warning signs of sleep apnoea/apnea
- Risk factors
- I think I might have sleep apnoea / apnea
- How are snoring and sleep apnoea / apnea treated?
- What is the outcome?
No signup is required. No credit card.
Nothing at all in fact.
We do this to help – because we can.
Introduction
If you’ve ever spoken to someone who snores, they joke about it:
“I’m ok, I can’t hear it!”
It’s a phrase we hear all the time.
In many cultures, snoring is humorous, and snoring noises are often used in film and animation to indicate that someone is sleeping… the irony being that the snorer might be only getting poor quality sleep, and indeed, snoring can be a symptom of something more serious.
In this Award-Winning Guide, we’ll give you an overview of snoring and sleep apnoea, to help you make the decision on whether ‘snoring’ is something you should address… because it might not be just snoring.
- Snoring isn’t YOUR problem – right?
- What are the benefits of treatment?
- When a sleeping problem becomes more serious
- What happens when you sleep?
- The warning signs of Obstructive Sleep Apnoea
- Risk Factors
- It might not be ‘just’ snoring…
- Effect on partners
- I think I might have sleep apnoea
- How are snoring and sleep apnoea treated?
- ‘Mouthpieces’ – Dental Devices
- Medicines
- Positive Airway Pressure (PAP) therapy
- Surgery
- What is the outcome of snoring and sleep apnoea?
- What next?
- Acronym Glossary
- Support Groups
- References


This invaluable Guide explains in easy-to-understand language what snoring and sleep apnoea is, why it is a problem to BOTH the snorer and partner, and what can be done about it.
It is MUST READ information for anyone with a snoring or sleepiness problem.
Snoring isn’t YOUR problem – right?
When people joke about snoring, it’s because it’s not the actual snorer’s problem… it’s the problem of the people who hear the snoring.
Actually, it could be everyones’ problem – only perhaps you don’t know it yet. As you become more of an advanced snorer with age and weight gain, your snoring may develop into obstructive sleep apnoea (OSA) and then your ‘snoring’ will disturb your own sleep more and more.
As the years go by, you will start to feel like you are suffering from a cross between a hangover and jetlag. All the time. In fact, you will probably have forgotten what it felt like to be truly alert… and that’s an issue, as it contributes to not recognising you might have a problem!
“That’s not me”, you might say, “and anyway, why should I care?”
Apart from the obvious i.e. less earache/bruised ribs (and remaining in the same bed as your partner) you might like to stop snoring so that should you fall asleep on public transport / flying or at work etc. you won’t have the accusatory looks on waking… Or you might like to go camping, take a short break or stay over at friends without ridicule.
These are perhaps some of the social (or avoiding anti-social) reasons, your rather tired partner will no doubt have already told you about.
So back to you, snoring IS potentially doing YOU harm. First off, the vibration in your throat from the floppy tissue waving in the breeze as you breathe (that’s what makes the noise) vibrates the arteries1 in your throat. While the jury is out on this one, it is thought to harden the artery walls, which isn’t so great.
So what is ‘sleep apnoea’?
It’s made up of apnoeic episodes. A sleep apnoeic episode is a silent period between snores.
This is when you can’t breathe. That’s a scary thought! Your chest and stomach continue to move up and down but no air gets in to your lungs.
You are in effect suffocating.
Your partner may have noticed one of these ‘episodes’ and nudged you to wake up and breathe… but then they go to sleep or leave the bedroom, whilst you keep doing this all night…
The worst bit is that you are going to feel absolutely exhausted. Tired as you have never experienced before.
This is because your sleep is poor quality and inadequate. It is fragmented. You are effectively just dozing all night, in short bursts, between the silent periods when you are not breathing.
In the day, you will be irritable and most likely unpleasant to know, as you crave rest. You may lose your sex drive and your daytime sleepiness, known as ‘hypersomnolence’ makes you a significant road traffic accident risk.
This daytime sleepiness is the chief symptom of what Doctors call: ‘Obstructive Sleep Apnoea Syndrome’.

Apnea or Apnoea?
You may see two spellings of apnoea. The US spelling of ‘apnea’ is used more widely than the UK spelling ‘apnoea.’

JARGON ALERT!
We mean OBSTRUCTIVE sleep apnoea when we say ‘sleep apnoea’.
Explained:
Obstructive = an obstruction (used to differentiate the problem from Central sleep apnoea).
Sleep = you are not awake when this happens.
Apnoea = cessation of breathing.
Put it all together and you have, in effect, self-suffocation when asleep!
Reference
1 LEE et al, (2008) Heavy snoring as a cause of carotid artery atherosclerosis.
Sleep. Sep;31(9):1207-13. PubMed PMID: 18788645; PubMed Central PMCID:
We mean OBSTRUCTIVE sleep apnoea when we say ‘sleep apnoea’.


JARGON ALERT!
Hypersomnolence could be described as ‘irresistible sleepiness in unsuitable circumstances‘.
Obstructive Sleep Apnoea SYNDROME is when your sleep apnoea starts to makes you sleepy in the day. This is known as symptomatic.
What are the benefits of treatment?
The benefits of treatment include:
- Better life expectancy
- Improved quality of life
- Greatly reduced risk of having a heart attack or a stroke
- Improve your blood glucose levels
- Avoid falling asleep while driving
- Wake up more refreshed in the morning – and without a headache
- Be more sharp and ‘on the ball’
- Be less irritable and combat depressive feelings
- Lose weight more easily
- Have more fun and enjoyment in life
- Have interest in and enjoy a better sex life
Hopefully, from the above list you can see that snoring, for both a snorer and their partner is more than an annoyance.
Not sleeping well, for whatever reason, can seriously affect your health and even your life expectancy.
Sleep is essential for the body and brain to repair and renew itself.
Chronic lack of sleep can contribute to a range of medical conditions, including:
- Obesity
- Diabetes (type 2)
- High blood pressure
- Heart disease
- Depression and anxiety


If you believe you have any of these conditions you should seek advice from your doctor or medical practitioner.
When a sleeping problem becomes more serious
Sometimes there are significant health issues that prevent people from sleeping well.
Sleep Related Breathing Disorders (SRBD) – these disorders are one of the most common problems that affect people’s sleep. One in five adults have some form of SDB.2 It can range in severity from simple, but disruptive snoring to sleep apnoea where you have stopped breathing.
- Snoring – the most common form of SRBD – the airway becomes restricted, causing the soft tissue to vibrate, making the snoring noise.
- Obstructive Sleep Apnoea (OSA) – where the airway closes so you stop breathing. Periods of no breathing may last for 10 seconds or longer and occur several hundred times a night.
- Central Sleep Apnoea (CSA) – a less common form of sleep apnoea which occurs when the brain fails to send the right signals to body to regulate sleeping.
There are a range of treatments that can effectively help people with SDB (and their partners) achieve a good night’s sleep. Snorer.com’s mission is to provide the information on how-to-choose, in an easy to read format in our Guides.

ACRONYM ALERT!
SRBD = Sleep Related Breathing Disorders has superseded the term SDB
Reference
2 YOUNG T, PEPPARD PE, GOTTLIEB DJ. (2002) “Epidemiology of obstructive sleep apnea: a population health perspective.”
Am J Respir Crit Care Med;165(9):1217-39.

ACRONYM ALERT!
SRBD = Sleep Related Breathing Disorders are a group of abnormal breathing patterns that occur while asleep.
What happens when you sleep?
As you sleep the muscles that control the upper airway relax. If the muscles relax too much, the airway becomes narrowed, limiting the airflow as you breathe. This may lead to:
- Vibration – which produces the snoring noise
- Collapse – where breathing stops altogether, called obstructive sleep apnoea (OSA)
The warning signs of Obstructive Sleep Apnoea (OSA)
There are a number of warning signs that may indicate if you are suffering from OSA.
During the night:
- Snoring followed by a period of silence and then perhaps a loud snort or gasp as you resume breathing
- Waking up at night with a sore throat
- Frequent need to get up and use the toilet
During the day:
- Waking up feeling unrefreshed or with a headache or sore throat
- Feeling excessively sleepy during the day
- Decreased energy and motivation
- Difficulty in concentrating
- Irritability

Risk factors
There are certain factors that may mean you are at greater risk from OSA:
- Being male!3
- Being overweight
- Being a heavy snorer
- A family history or snoring and sleep apnoea
- Drinking alcohol in the evening
- Smoking
- Silent pauses in-between snores could be a sign of Obstructive Sleep Apnoea (OSA)
Reference
Obstructive Sleep Apnoea affects men more than women. “…men had a prevalence of 3.9% and women 1.2%”.
3 BIXLER, E et al, “Prevalence of Sleep-disordered Breathing in Women”
American Journal of Respiratory and Critical Care Medicine, Vol 163, No 3 (2001), pp 608-613.
It might not be ‘just’ snoring…
Read on to find out why it’s bad…
The effect of (OSA) on your body
When you are asleep, if your airway becomes blocked you may stop breathing. If it occurs for 10 seconds or longer, it is considered an ‘apnoeic event’. It can happen frequently – sometimes hundreds of times a night.
Stress on your body
If you stop breathing this places a stress on your brain and your heart as they both struggle to work with the lack of oxygen.
Disrupted Sleep
Your brain wakes you up in order to start breathing again and so your sleep is disrupted over and over again.
Impact on your health
Stress on your brain and heart, coupled with disrupted sleep have serious effects on your health. Left untreated, they are a contributing risk factor in high blood pressure, heart disease, stroke, diabetes, and depression.
- More than 35% of people with sleep apnoea suffer from high blood pressure, increasing their risk of heart disease.4
- 83% of people who continue to suffer from high blood pressure despite taking three or more drugs, also have sleep apnoea.5
- Almost 70% of people who’ve had a stroke have sleep apnoea.6
- A person with sleep apnoea is seven times more likely to have a car accident.7
Effect on partners
It is not just people with OSA or a snoring problem whose health can be affected. Partners, whose own rest is continually disturbed, may also suffer the effects of chronic interrupted sleep.
I think I might have sleep apnoea…
If you are concerned that you may have sleep apnoea, visit your Doctor/Primary Care Physician. They may then refer you to a sleep laboratory for tests. A sleep laboratory is run by a respiratory physician/pulmonologist or perhaps a neurologist. In both cases, they are often supported by specialist staff known as Registered Polysomnographic Technologists (RPSGT).
The sleep laboratory will then determine if a ‘home sleep test’ is required or ask you to come in overnight for a polysomnogram (PSG). To explain ‘somnogram’ means sleep test and ‘poly’ means lots – in that lots of readings are taken at the same time as you sleep!
How are snoring and sleep apnoea treated?
Some causes of snoring are the result of lifestyle habits. By altering these habits, you may be able to minimise your snoring.
Try these ideas below as a start:
- Always try to sleep on your side, instead of your back.
- Avoid alcohol in the evening.
- If you smoke – stop. The smoke inflames the soft tissue of your throat and makes the airway narrower.8
- Attempt to keep your body in alignment. This should be done by raising the head of the bed itself or by making sure that your pillow is at the correct height.
- Try to maintain a healthy diet and weight. Aim to eat five servings of fruits and vegetables in your daily diet.
- Prepare meals in a healthy way, for example baking or grilling foods instead of frying. This will not only reduce the amount of fat in your throat tissues, but will also help improve your general health.
- Talk to your doctor about your ideal target weight, and it may be appropriate to consult your Doctor before taking part in any exercise.
- Regular exercise will improve muscle tone and in turn may reduce your incidence of snoring. If you are starting out from no exercise, consult your Doctor before taking part in any exercise. They may suggest beginning with a 10-minute period of light exercise and gradually build from there. When you are ready, it is recommended that you exercise at least three to four times a week. Try to work up to 20–30 minutes a session.
References
4 PAGEL, J. et al. (2008) “Obstructive Sleep Apnea: Recognition and Management in Primary Care.” Supplement to The Journal of Family Practice. Vol. 57.
No. 8.
5 WORSNOP et al. (1998) The prevalence of obstructive sleep apnea in hypertensives. American Journal
of Respiratory Critical Care Medicine; 157:111-5.
6 BASSETTI et al. (1999) Sleep apnea
in acute cerebrovascular diseases: final report on 128 patients. Sleep;22:217-223
7 HORSTMANN et al. (2000) Sleep related accidents in sleep apnea patients. Sleep.
Reference
8 WETTER, D W et al; “Smoking as a Risk Factor for Sleep-Disordered Breathing”
Arch Intern Med. (1994); 154(19):
2219-2224.

‘Mouthpieces’ – Dental Devices
If your doctor considers a ‘mouthpiece’ could be an effective treatment option for you then we suggest you read the Snorer.com Guide How to choose a ‘Mouthpiece’ [new tab]
Buying an anti-snoring mouthpiece that you can fit yourself sounds simple and straight forward. However, as with most simple things, it is a little more complicated than it at first appears. There are serious problems with self-diagnosis and self-treatment. The lay person may appreciate that he/she snores but may be totally unaware of a potentially serious underlying medical condition which may be the primary cause of the snoring.
Therefore, without correct assessment, diagnosis and treatment, the patient may be doing himself/herself more harm than good, in perhaps ‘treating’ the symptom of snoring, and missing a more serious disorder.
There is much more about ‘mouthpieces’ for snoring and sleep apnoea in the Snorer.com Guide: How to choose a ‘Mouthpiece’ [new tab]

A diagnosis can only come from a medical professional and doesn’t mean a ‘self-diagnosis.’

JARGON ALERT!
MRD (Mandibular Repositioning Device)
MAS (Mandibular Advancement Splint)
Mouthpiece, ‘Gumshield’, Oral Appliance, Device, Splint…
These are different names for the same thing: a device worn in your mouth, which holds your lower jaw forwards, to help you breathe better while asleep.
Medicines
If you have allergies that cause nasal congestion, try an oral or spray decongestant available from your chemist. If your nasal congestion doesn’t clear up in a few days, see your doctor as you may need stronger medication, or other measures to clear your nasal passages.
If your nasal congestion is caused by a structural problem in the nose such as a deviated septum, there are surgical techniques that can correct it.

JARGON ALERT!
The nasal septum means the ‘wall’ that separates the nostrils of the nose in the nasal cavity (not the bit that you can see).
Positive Airway Pressure (PAP) therapy
If your doctor diagnoses sleep apnoea and none of the simple remedies are successful, he/she may recommend using positive airway pressure therapy (PAP). This involves wearing a mask over your face while you sleep, to force air through your nose (and sometimes mouth as well). This prevents the airway from closing when you breathe in.
There are several manufacturers of PAP and it is considered the best solution for severe sleep apnoea. However, some people find wearing a mask in bed every night difficult to tolerate. Overcoming the difficulties using PAP are a focus for the competing companies and features such as improved mask design, warming and humidifying the air, raising the air pressure from a low level as you fall asleep and varying the air pressure as you breathe in and out are all fairly recent advances.
More in the Snorer.com How to Choose PAP therapy Guide. [new tab]
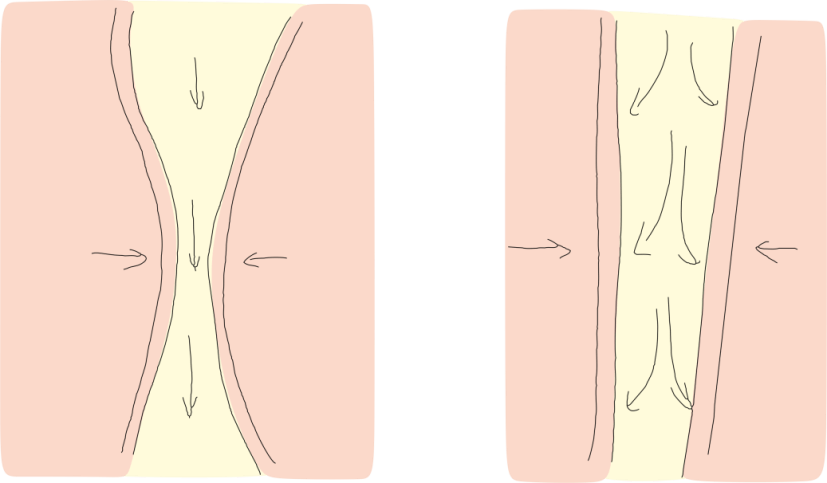
LEFT: The impact of a narrowing airway on the air you breathe. The air has to travel faster as the airway narrows. If the airway narrows sufficiently to reduce airflow, it is a hypopnea. If it collapses on itself, it causes an apnoea.
RIGHT: How increased air pressure holds (or splints) open the airway.
Surgery
While making lifestyle changes should be the first step in treating your snoring, these measures are not always effective. If that is the case, whilst surgeries are rarely performed, there are surgical options.
You might have heard of a form of surgery called laser-assisted uvulopalatoplasty (LAUP). This relatively new procedure assumes that the snoring noise is created by the soft palate (occasionally the back wall of the throat). A small probe is inserted into the area to be reduced and for want of a better word the tissue is ‘microwaved’ this reduces the bulk and stiffens the tissue.
Radio-frequency ablation – sometimes known as Somnoplasty® reduces the size and amount of soft tissue in localised areas. It may have a short term effect on snoring – however repeated operations are generally necessary and individuals may be reluctant to undergo a second (of perhaps many more) operation after experiencing the first.
In general, this surgery does not have serious side effects and you can continue your regular activities immediately after the procedure. In some cases, surgery can raise or lower the pitch of the voice. Before you decide on surgery, talk it over with your doctor. Surgical options for sleep apnoea are not recommended – apnoea responds better to PAP.
However, if your sleep apnoea is caused by a jaw deformity, an operation to correct the deformity (Osteotomy) may be performed. This is successful in most people.
Historically, surgery known as a uvulopalatopharngoplasty (UVPPP) was performed. However, due to the low success rate it is no longer offered.
If your sleep apnoea is caused by large tonsils and/or adenoids, these can be removed with an operation called a tonsillectomy or adenoidectomy. This is not a trivial operation as an adult.
There is much more about surgical options for snoring and sleep apnoea in the Snorer.com Surgical Guide. [new tab]

JARGON ALERT!
Radio-frequency ablation is a method of removing tissue within the body by a minimally invasive procedure – which means a procedure that is less invasive than open surgery.

JARGON ALERT!
Osteotomy is a surgical procedure where bone is cut: https://www.snorer.com/jargon-buster/

JARGON ALERT!
Uvulopalatopharyngoplasty (UVPPP) refers to surgical removal or reduction of the uvula (dangly bit at the back of the throat) and portions of your soft palate.

JARGON ALERT!
Tonsillectomy is where the tonsils are removed. Adenoidectomy is where the adenoids are removed. More information is in the Snorer.com Jargon Buster! https://www.snorer.com/jargon-buster/

JARGON ALERT!
Find out more about other Snorer.com Guides at: https://www.snorer.com/information-guides/
What is the outcome of snoring and sleep apnoea?
Snoring is an annoyance for most people, but for those who snore habitually, it can cause serious social and marital discord. Sometimes it can be remedied by lifestyle changes and/or surgery however a mouthpiece in certain circumstances may be considered a safe non-surgical option which may be considered as a first step.
Sleep apnoea is a more serious condition that can cause chronic illness and has been linked to earlier death when linked with other conditions such as heart disease, but several effective treatment options are available.
What next?
You might like to read the other Snorer.com Guides:
A diagnosis can only come from a medical professional and doesn’t mean a ‘self-diagnosis’ followed by ‘self-treatment.’
Find out more about other Snorer.com Guides at: https://www.snorer.com/information-guides/
Acronym glossary
• LAUP = Laser-assisted uvulopalatoplasty
• MAS = Mandibular Advancement Splint
• MRD = Mandibular Repositioning Device
• OSA = Obstructive Sleep Apnoea
• PAP = Positive Airway Pressure
• SDB = Sleep-Disordered Breathing
• SRBD = Sleep Related Breathing Disorders
• UPPP = Uvulopalatopharyngoplasty
Support groups
United Kingdom
• Sleep Apnoea Trust Association: http://www.sleep-apnoea-trust.org/
• Scottish Association for Sleep Apnoea (SASA): https://scottishsleepapnoea.co.uk/
• Irish Sleep Apnoea Trust: https://www.isat.ie
• Hope2Sleep: www.hope2sleep.co.uk
United States
• American Sleep Apnea Association: https://www.sleepapnea.org/
References
1. LEE et al, (2008) Heavy snoring as a cause of carotid artery atherosclerosis. Sleep. Sep;31(9):1207-13. PubMed PMID: 18788645; PubMed Central PMCID: PMC2542975.
2. YOUNG T, Peppard PE, Gottlieb DJ. (2002) Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med;165(9):1217-39.
3. BIXLER, E., et al, (2001) Prevalence of Sleep-disordered Breathing in Women. American Journal of Respiratory and Critical Care Medicine, Vol 163, No 3, pp 608-613.
4. PAGEL, J., et al. (2008) Obstructive Sleep Apnea: Recognition and Management in Primary Care. Supplement to The Journal of Family Practice. Vol. 57. No. 8.
5. WORSNOP et al. (1998) The prevalence of obstructive sleep apnea in hypertensives. American Journal of Respiratory Critical Care Medicine; 157:111-5.
6. BASSETTI et al. (1999) Sleep apnea in acute cerebrovascular diseases: final report on 128 patients. Sleep;22:217-223
7. HORSTMANN et al. (2000) Sleep related accidents in sleep apnea patients. Sleep.
8. WETTER, D.W. et al (1994) Smoking as a Risk Factor for Sleep Disordered Breathing. Arch Intern Med; 154 (19): 2219-2224
Legal statements
All trademarks are owned by their respective companies and acknowledged.
Meet the team behind the Guide at the BMA Awards Ceremony in London.
From left to right:
Kath Hope, Prof. Adrian Williams FRCP, Adrian Zacher, Emma Easton.
Please take a moment and write a review, to help others find useful resources. Thanks!

Created by Adrian Zacher | Page last updated 8th March 2022

