Pharmacy teams, Help People Stop Snoring!
Train to screen ‘snorers’ and signpost appropriately.
Do this free, evidence-based short course, to learn how to help:
How to get free online CPD:
Carry on from where you were (resume)
Button will show when you are logged in and enrolled.
Existing enrolled users:
Snorer Pharmacy® registered users:
Rated 5/5 based on 6 customer reviews
How do I begin?
First, enrol on the free (no obligation) online training course.
Once successfully completed, you may join Snorer Pharmacy: the pharmacist-led Snoring and Sleep Apnoea Service (subject to contract and an SOP).
Training is completely free and without any obligation.
When you’ve successfully completed the training, you will gain a digital course certificate (3 valuable CPD hours).
We charge should you opt to:
- Use our proprietary software tool
- Provide home sleep apnoea testing
We use a Pay-Per-Use pricing model, where you only pay when you have a customer. We consider that fairer.
As you would imagine, a contract and SOPs apply.
Get in touch and we can set up a time to discuss on the phone or via most video meeting apps.
We estimate the online course will take ~ 3 hours to complete.
Further reading is highly recommended, and should you choose, you can expect to spend some time becoming familiar with the signposting software (we consider this intuitive).
And (again should you choose) the Home Sleep Apnoea Testing equipment (not necessary for every patient).
Absolutely!
Drop us an email [contact@snorer.com] and we can setup a time that suits us both.
Look forward to speaking with you.
🙂

Our contact details
WhatsApp: 07769 187168
email: contact@snorer.com
Registered office:
4 Waterford Lane
Cherry Willingham
Lincoln
LN3 4AL
United Kingdom

Why do Anything About Snoring?
Obstructive Sleep Apnoea
30 sec video to explain WHY
My intention with Snorer Pharmacy® is to help you, the community pharmacy team, help patients with suspected sleep disorders, at the earliest possible opportunity.
The course is completely free, with no annoying adverts, no payment cards are required, and it’s provided without any obligation.
Please find the time (about 3 hours).

“Pharmacies are often the first port of call for snorers, or their desperate domestic partners.”
Alan Nathan, Pharmaceutical Journal.2
There is little, if any, evidence to support OTC ‘snoring’ products place on the market. But within the context of concurrent cardiovascular, obesity and T2DM epidemics, it might perhaps be forgivable to consider ‘snoring’, an irrelevance.
However, when you appreciate that metabolic syndrome is exacerbated by obstructive sleep apnoea (OSA)1 – a symptom of which is snoring, you may wish to reconsider.
Indeed, snoring without OSA is far from benign.
The social consequences alone:
- Sleeping apart
- Relationship disharmony
- No holidays because of enforced sleep disruption when sharing a hotel room
- Fear of travelling due to concern over falling asleep during long journeys on public transport and the consequent ridicule and embarrassment
mean snorers deserve valid help.
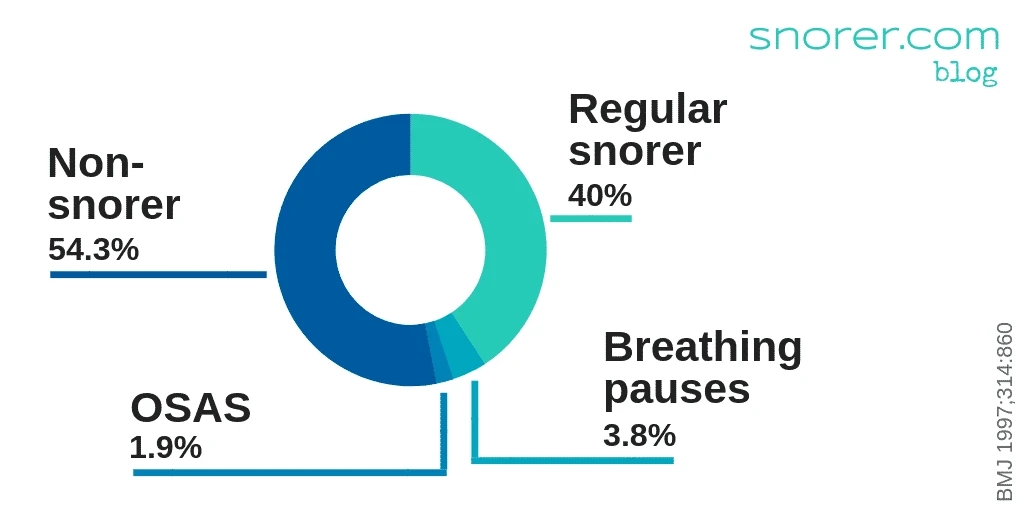
With an estimated 40% of the UK population reporting regular snoring3 this is a sizeable problem.
Snoring is commonly trivialised and sales of OTC snore ‘cures’ that encourage the unwary to self-diagnose and self-treat (in order to profit from their misery) commonplace.
Yet the snorer with untreated sleep apnoea can expect to:
Die 20 up to years sooner4
Finn L, Young T. Sleep Disordered Breathing and Mortality: Eighteen-Year Follow-up of the Wisconsin Sleep Cohort. Year Pulm Dis. 2009;2009:291-292. doi:10.1016/s8756-3452(08)791813
than the average lifespan, independent of age, sex and BMI, which is disappointing when diagnosis and treatment is available from the NHS, that could significantly extend their healthy life.
Screening and signposting for sleep apnoea are fulfilling roles for the community pharmacist that support the healthy living and better care agenda5.
Sleep apnoea is more common than you may think, perhaps as many as one in ten middle-aged men have it.6 Obstructive Sleep Apnoea Syndrome (OSAS) patients who receive treatment will be more productive, more motivated and live longer, healthier lives.
Our Unique Offering
Consists of three integrated elements:
Our free, online snoring course for UK pharmacy teams is divided into three chapters, each with a short assessment.
The final examination has a minimum pass mark of 80% to satisfy planned learning CPD requirements and to ensure pharmacy teams are educated sleep professionals.
Our turn-key online service for Community Pharmacy teams helps you signpost ‘snorers’ appropriately.
Our proprietary Snorer.me Signposting™ software is a UKCA marked Clinical Decision Support System (CDSS) utilising industry recognised pre-treatment screening tools.
We do NOT make/sell treatment devices. We have no vested interest in the outcome of signposting.

Snorer.com ranks on Google’s first page for commonly searched for snoring keywords and phrases.
We direct snorers and their long-suffering partners to consult a pharmacy team (or their GP).
How Does it Work?
Three Steps to Heaven-ly Sleep for your patients:

Learn about sleep & breathing and evidence-based care
YOUR EDUCATION
Integrate the latest evidence into decision making for snoring and sleep apnoea patients

Screen and recognise snorers with sleep apnoea symptoms
THEIR ENLIGHTENMENT
Identify at risk patients using our evidence-based software tool (Snorer Pharmacy®)
in line with the most up to date NICE guidelines

Signpost appropriately utilising your new knowledge
THEIR EMPOWERMENT
Incorporate patient-centred considerations when making clinical recommendations based upon recognised protocols
Why we do this
And why you should too:
GPs cannot make dental appliances (first-line therapy for benign, anti-social snoring). While a dentist cannot refer a patient directly to a hospital for further investigation into their hypersomnolence.
Pharmacists are therefore well-placed to signpost patients appropriately. Directing them to the most appropriate care pathway based upon their symptoms and medical history.
In the (13 mins) video below, Adrian Zacher takes a ‘Deep Dive’ into the developing role of the sleep-trained pharmacist:

What does Signposting look like?
Double speed!
ABOUT US
Our Story
Adrian Zacher established Snorer.com after 18 years in the sleep industry.
Initially, Adrian was satisfied just to disrupt the pseudo-scientific marketing, commonly used to exploit snorers and their partners.
This grew into creation of our online signposting software and comprehension that pharmacy teams are the appropriate professionals to deliver it.
Snorer.com is proudly independent of any sleep business and NOT part of an affiliate scheme.
What Can Pharmacists do to Advise Snorers?
Screening, Recognising and Signposting
An abundance of Over-The-Counter (OTC) products for snoring exist.
However, they generally have little, if any, objective evidence of effect.

In our Snorer.com blog, we independently review ‘cures’ for snoring and sleep apnoea.
As a sleep-trained pharmacy team member you will be able to advise snorers in a more informed way.
Once trained, you will be able to:
- Recognise OSA symptoms that merit further investigation
- Use our signposting tool (Snorer Pharmacy®) to:
- Assess snoring and contributory factors
- Screen and connect patients to NICE recommended treatment6, for both anti-social snoring and sleep apnoea
- Discuss evidence-based help that may extend their healthy life
- Use our home sleep apnoea testing service to improve the patient’s likelihood of onward referral to secondary care, and potentially reduce their time to treatment
Signposting ‘snorers’ to appropriate care pathways is a key role for the pharmacist 7.
Does the Evidence Support the Pharmacists’ Sleep Role?
A Public Health Benefit
In a systematic review of pharmacists performing OSA screening services8 the authors observed that:
“Pharmacists are the most accessible and underutilized healthcare resource in the community and can have a significant role in screening patients for OSA.”

Thus, it could reasonably be argued a Public Health benefit, for pharmacists to recognise snorers with symptoms of Obstructive Sleep Apnoea Syndrome (OSAS) and particularly where those patients have relevant history and/or comorbidities e.g.:
- T2DM (type II diabetes mellitus)
- Obesity
- Hypertension (high blood pressure)
- CVD (heart disease)
- CVA (stroke)
Such comorbid snorers should be referred to their GP1 with comprehension that referral uptake may be poor if left to the individual to action,9 ideally a note made on the patient’s Electronic Health Record or Summary Care Record for the GP’s attention10.
Current NICE Guidelines7 state that mandibular advancement devices (custom-made, prescription ‘mouthguards’) are first-line therapy for snoring and mild OSA, when the snorer is not drowsy during their normal awake time (hypersomnolent) and has no relevant comorbidities.
Such patients should be directed to a sleep-trained dentist, for the dentist to determine the patient’s suitability for a custom-made, prescription mandibular advancement device.
Our online ‘pharmacist driven’ signposting tool11 (Snorer.me Signposting™) gives you the option of referring those you have screened as not needing further investigation, to our network of sleep-trained dentists. Particularly useful when a GP referral would be unlikely to result in a secondary care referral and serve only to:
Unnecessarily consume GP clinical time
Waste the snorer’s time
And in the worse case scenario, unnecessarily consume diagnostic capacity in secondary care
We created our signposting tool (CDSS) to develop the primary care network, and connect snorers to pharmacists so they may accelerate sufferers to valid, evidence-based and effective treatment.
Benefits & Outcomes
Benefits:
The snorer has been:
- Assessed by a sleep-trained professional
- Screened for symptoms of OSA
- Signposted appropriately
Outcomes:
The snorer knows:
- Why they snore
- What to do about it
- Where to go to stop
The patient now has a comprehensive, actionable, personal report.
They have been accelerated to the most appropriate care.
Why Work With Us?
Start Now
Make a difference to snorers’ and partners’ lives:
What Others Say

Sleep-trained pharmacist review
Course review for Snoring and Obstructive Sleep Apnoea for the Pharmacist
Gareth Evans, Pharmacist of the year 2023
Thank you for the opportunity to train as a sleep trained pharmacist. Your training platform was simply superb – well thought out, engaging and highly informative for all things snoring and OSA. I can’t wait to utilise my new-found knowledge and help the many people out there lead a healthier life. In fact now that I know how important this field is I may even save a few lives in the process. Thank you again and I hope every pharmacist takes up this opportunity!!
Start Now
Make a difference to snorers’ and partners’ lives:
References
- IDF. Consensus Statements. Int Diabetes Fed. 2008;51(5):i-ii. oi:10.1159/000480305 ↗ Accessed January 14, 2020.
- Snoring and the evidence behind the various treatments available Pharmaceutical Journal, Feb 2010 ↗ Accessed 15th Oct 2020.
- Ohayon MM, Guilleminault C, Priest RG, Caulet M. Snoring and breathing pauses during sleep: Telephone interview survey of a United Kingdom population sample. Br Med J. 1997;314(7084):860-863. doi:10.1136/bmj.314.7084.860 https://pubmed.ncbi.nlm.nih.gov/9093095/ ↗ Accessed January 14, 2020.
- Finn L, Young T. Sleep Disordered Breathing and Mortality: Eighteen-Year Follow-up of the Wisconsin Sleep Cohort. Year Pulm Dis. 2009;2009:291-292. doi:10.1016/s8756-3452(08)79181-3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2542952/ ↗ Accessed January 14, 2020.
- Pharmacy in England: Building on Strengths – Delivering the Future – Great Britain. Department of Health – Google Books. ↗ Accessed January 14, 2020.
- OSA estimates for the UK (2019) https://osapartnershipgroup.co.uk/clinicians/osa-partnership-group-clinicians-osa-estimates-for-the-uk ↗ Accessed 12th March, 2021.
- NICE CKS. Obstructive sleep apnoea syndrome. Clinical knowledge summaries. https://cks.nice.org.uk/obstructive-sleep-apnoea-syndrome ↗ Accessed 30th June 2020.
- Cawley MJ, Warning WJ. A systematic review of pharmacists performing obstructive sleep apnea screening services. Int J Clin Pharm. 2016;38(4):752-760. doi:10.1007/s11096-016-0319-0 https://link.springer.com/article/10.1007/s11096-016-0319-0?shared-article-renderer ↗. Accessed January 13, 2020.
- Fuller JM, Wong KK, Grunstein R, Krass I, Patel J, Saini B. A Comparison of Screening Methods for Sleep Disorders in Australian Community Pharmacies: A Randomized Controlled Trial. Baradaran HR, ed. PLoS One. 2014;9(6):e101003. doi:10.1371/journal.pone.0101003 https://pubmed.ncbi.nlm.nih.gov/24978952/ ↗ Accessed 30th June 2020.
- Summary Care Record (SCR) in community pharmacy – NHS Digital. https://digital.nhs.uk/services/summary-care-records-scr/summary-care-record-scr-in-community-pharmacy ↗. Accessed January 13, 2020.
- Zacher A, Easton E. P076 Signposting for snoring: does it optimise use of GP time? Online surveys of patients and sleep-trained dentists. BMJ Open Respir Res. 2019;6(Suppl 1):A47-A48. doi:10.1136/bmjresp-2019-bssconf.76 https://bmjopenrespres.bmj.com/content/6/Suppl_1/A47.2 ↗ Accessed 30th June 2020.
Snorer Pharmacy® is a registered trademark.
Snorer.me Signposting™ is a UKCA marked clinical decision support system (CDSS) software as a medical device (SaMD).
The manufacturer is Snorer.com Ltd. |Page created by Adrian Zacher. All rights reserved. Copyright 2020-2025. | Last updated 14 April 2025.

